 Health systems and providers are always looking for ways to better manage and more effectively communicate with high-risk patients to improve their clinical and economic outcomes.
Health systems and providers are always looking for ways to better manage and more effectively communicate with high-risk patients to improve their clinical and economic outcomes.
For patients who are clinically in a high-risk category, it can be difficult to predict whether they are moving closer to or further away from their next hospital readmission.
The challenge often comes down to the systems themselves—what patient data they contain, how much predictive intelligence they can produce, and how well they facilitate interpersonal communication with high-risk patients.
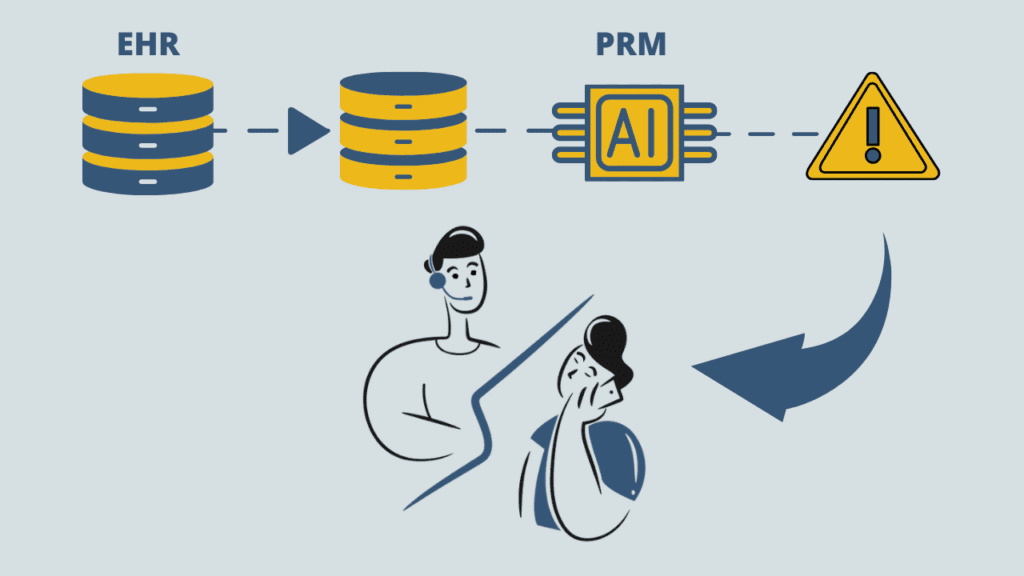
Clinical systems such as EHRs are designed to manage a patient’s clinical data. However, clinical data points alone are not a reliable predictor of future utilization. In other words, using just clinical data may paint an overly optimistic or pessimistic picture. Clinical liaison teams need additional non-clinical data points at their disposal in order to have a full, 360-degree view of each high-risk patient.
With a patient relationship management system like Salesforce Health Cloud that presents an array of clinical and non-clinical information to a member of the patient liaison team, that person can make more informed decisions about what actions to take with an at-risk patient.
The Role of AI
Over time, artificial intelligence can learn what combination of risk factors is most likely to result in readmission.
The larger the array of data points across the care continuum, the broader the knowledge base the AI can assign a predictive score from to each patient. This score is used to indicate a patient’s relative level of risk for near-term readmission.
Patient stratification tiers can be based on ranges of scores, such as 71 – 80, 81 – 90, and 90 – 100.
If, for example, a patient’s risk score suddenly jumps into the top strata, staff can be altered by email or via an in-app bell notification.
This scoring mechanism helps staff focus on specific at-risk patients with whom they can then exercise human judgment on to figure out next steps. Of course, liaison staff can make decisions completely outside of anything that AI suggests.
Let’s look at the clinical and non-clinical data points that, in aggregate, can contribute to a patient’s risk level.
Clinical Data Points For High-Risk Patients
Common EHR data points can be made available in a patient relationship management system through integration technologies, such as a FHIR Gateway.
Diagnoses
High-risk patients, by definition, have at least one high-risk diagnosis. They may also have high-risk comorbidities. Diagnostic data represents accurate, current information from an EHR system about diseases and other conditions.
Demographics
A key demographic indicator is a patient’s age. Knowing whether a patient is in their 20’s or in their 60’s can influence how an at-risk patient is scored for risk.
Repeat visits
Many high-risk patients will make at least one visit to the ER within 30 days of discharge. Being able to view the volume of repeat visits can help liaison teams get ahead of potential readmissions.
A recent readmission
EHR data reports whether a patient was readmitted to the hospital within the last month, for example.
Prescribed medications
It’s important for liaison teams to know what medications a high-risk patient is taking. High-risk patients may be on medications for high blood pressure, cholesterol, or mental illness.
Tests & test results
High-risk patients can also be high utilizers of imaging studies, MRIs, CT scans, and certain types of lab work.
Immunization dates
An absence of immunizations for infectious diseases such as COVID-19, hepatitis B, and shingles can factor into risk for readmission.
Non-Clinical Data Points for High-Risk Patients
Now we come to the type of information that is not necessarily contained within an EHR but which is important for managing high-risk patients.
Social Determinants Of Health (SDOH) are inputs that mainly need to be gathered from home and other non-clinical settings.
Adherence to prescribed medications
Low adherence may not be apparent in clinical data. The EHR may report that the patient has filled prescriptions, but the EHR will not be aware that the medicine is not being taken as prescribed.
Much of this information can only be gleaned from a conversation or an email exchange with a patient or a patient’s family member.
Level of family support
Family members can both support the patient directly and give liaison staff a more accurate real-time picture of the patient’s current situation.
The patient’s living situation
The EHR’s current billing address may not be the patient’s current living address. Is the patient experiencing homelessness? Is the patient living under a roof but constantly moving from one location to another?
Substance abuse profile
While there may be clinical information that relates to substance abuse, a patient’s family member and other people in a patient’s life can be a better source of current information about the patient than the most recent EHR progress notes.
Best practices and recommendations
In any health system, there is a need to foster a common set of best practices among those responsible for engaging with at-risk patients
Beyond the data analysis, there are various features in a patient relationship management system like Salesforce Health Cloud that ensures greater consistency as to how high-risk patients are managed.
Flows (guided visual experiences), validation rules, and in-app guidance are just a few of the factors that can drive consistency in working with patients.
J2 Interactive is an award-winning software development and IT consulting firm that specializes in customized solutions for healthcare organizations.
If you’d like to learn more about Salesforce Health Cloud & AI for working with high-risk patients, please fill in our Contact Us form or let Otis The Chatdog know that you want to speak to an expert.




