Updated: October 21, 2019
 Post acute care continues to be a rapidly growing segment within healthcare. The growth has been driven both by economics and by technological innovation.
Post acute care continues to be a rapidly growing segment within healthcare. The growth has been driven both by economics and by technological innovation.
On the economics front, insurance companies and Medicare have reduce reimbursements for readmissions that occur shortly (10 – 31 days) after a patient has been discharged.
Beginning in October 2012, the Hospital Readmissions Reduction Program required the Centers for Medicare and Medicaid Services (CMS) to reduce payments to inpatient prospective payment system (IPPS) hospitals with excess readmissions.
Insurance companies have explicit readmission policies which can limit reimbursements under certain circumstances.
Along with the shift to post acute care, more effective treatment outside of an acute care facility has been possible. This is in part due to a myriad of technological advances.
When a patient is discharged from an acute care facility, there are several possible paths that can be taken. Home health care is one. Inpatient rehabilitation is another. The latter often precedes the former.
Acute inpatient rehabilitation facilities
These are also known as long term acute care (LTAC) centers. For many patients, an LTAC represents a transitional period before a return to their home. The average length of stay is about 25 days.
A stay at an LTAC can be required in the case of conditions such as burns, internal organ injuries, brain injury, heart attack and stroke. It may take weeks after discharge from an acute care facility before a patient is determined to be well enough to return home.
An example of this type of facility is Alta Bates in the San Francisco Bay Area. In Massachusetts, the Spaulding Rehabilitation Network has locations across the state.
Post acute care at home
In many cases, a patient may go directly from an acute care facility to post acute care in the home.
An example of this is post acute orthopedic care, after an injury or elective surgery. The patient’s vitals signs are stable and within normal limits, so the patient can return home. However, the patient may need in-home assistance from a physical therapist with early stage physical rehabilitation. The patient may need pain medication administered by a nurse.
A stroke patient is another example. The patient may be able to go directly home from an acute care facility but needs in-home physical therapy, occupational therapy and/or speech therapy.
Depending upon a patient’s needs, a variety of healthcare professionals can be available for home visits, including:
- Nurses
- Physical therapists
- Occupational therapists
- Speech-language pathologists
- Home health aides
- Social workers
On several different levels, technology has made home health care a more viable and an earlier option for many patients. Let’s look at three of these areas.
- Portable medical devices and equipment
- Monitoring of a patient’s physical movement (or lack thereof)
- Patient information, personalized care plans, scheduling & dispatch
1. Portable medical devices and equipment
A greater number of portable medical equipment options is one of the factors has allowed for more quickly transferring a patient from an acute care facility or post acute care facility to the home. Here are some of the categories:
- Medication administration equipment
- Test kits (blood or urine)
- First aid equipment
- Assistive technologies (sensory abilities, mobility)
- Durable medical equipment (beds, lifts)
- Meters and monitors (blood pressure, heart rate, glucose levels)
- Treatment equipment (medical therapy administration)
- Respiratory equipment
- Feeding equipment
- Voiding equipment
- Telehealth equipment (for collection and transmission of data)
With the proliferation of home care equipment and devices, manufacturers have had a growing responsibility to recognize and mitigate hazards. Increasingly, manufacturers are relying on technology to get direct feedback from patients.
2. Monitoring of a patient’s physical movement (or lack thereof)
There several ways that an in-home patient can be monitored for any irregularities in movements such as falls—or exceptions to routines such as a failure to access food locations.
There are a variety of devices that can detect falls and generate an alert to a call center agent. The agent can then communicate directly with the patient.
Video Monitoring
Devices like the Nest Cam home camera can be used to monitor activity, especially of the elderly.
Personal voice assistants
A personal voice assistant such as Amazon Echo or Google Home can be set to audit for certain phrases. A distressed in-home patient can speak a command to “wake up” a voice assistant and then verbally relay the issue to a home care provider.
Sensor monitoring
A less intrusive form of monitoring than video or audio is sensor monitoring. Sensors can be placed at different locations within the home to ensure that regular activity is taking place.
3. Patient information and personalized care
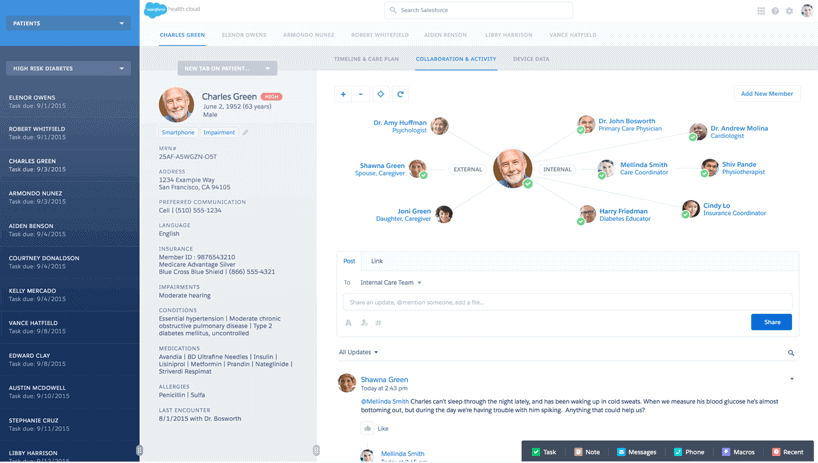
CRM technologies such as Salesforce Health Cloud have made many facets of a patient home care relationship easier to manage.
Patient information
Patient data and health information can be centrally stored and securely accessed by a home care professional from a laptop, a table or a mobile phone.
Health Cloud can also be used to house information about contacts who are around the patient. Contact related to the patient can include physicians, at-home caregivers and emergency contacts.
Care plans
With Health Cloud, one or more care plans can be developed for an in-home patient. A plan can include what type of healthcare professional should be at the patient’s home and on what schedule. Details about physical therapy exercises, when wound dressings should be changed and what medication should be administered can be included in a care plan.
Dispatch of healthcare professionals
The field service component of Salesforce Health Cloud is used to dispatch the right healthcare professional to the home at the right time. Time spent at the patient’s home can also be tracked. Integration with applications such as Google Maps can determine the needed travel time between homes. Care team members can securely access Health Cloud data on mobile devices.
Centralization of data collected from monitoring devices
Data collected from one or more monitoring devices can be stored within the patient’s Health Cloud record. That makes the information more easily accessible by a physician and any professionals who are dispatched to the patient’s home.
Personal voice assistants
 Now that Amazon’s Alexa has HIPAA-compliant skills, there are a number of potential interfaces with a CRM system such as Salesforce Health Cloud.
Now that Amazon’s Alexa has HIPAA-compliant skills, there are a number of potential interfaces with a CRM system such as Salesforce Health Cloud.
These include: scheduling appointments; receiving reminders about upcoming visits from care givers; accessing post-discharge instructions.
Provide More Effective Post-Acute Home Care With Salesforce Health Cloud
 J2 Interactive is a Salesforce Silver Consulting Partner. Our Salesforce group focuses exclusively on solutions for healthcare and life sciences organizations.
J2 Interactive is a Salesforce Silver Consulting Partner. Our Salesforce group focuses exclusively on solutions for healthcare and life sciences organizations.
To discuss how Health Cloud can work for your organization, please get in touch with us.