| Week One Summary | Week Two Summary | Week Three Summary | Week Five Summary |
|---|

2020 marks the sixth year of SHIEC and the first year of it going virtual! Join us over the next five weeks from August 17 – September 15 as we recap the 10-day series of virtual sessions!
A Community Driven Approach to Move Upstream and Address the Social Determinants of Health

- Date: Tuesday, September 8, 2020
- Presenter: Taylor Justice, Co-Founder & President, Unite Us
- Overview: Unite Us co-founder and president Taylor Justice explained the needs that guided his company into becoming an operating system for social care, highlighting his company’s role in helping HIEs identify and incorporate Social Determinants of Health (SDOH) into their services.
Taylor Justice had been a volunteer for a non-profit organization supporting military veterans transitioning from active service into communities. The organization for which Justice volunteered was like many—one that relied on spreadsheets and a collection of resource listings, updated periodically, to track their clients’ needs and what resources were available to them. Processes tended to be very manual, and Justice noticed that much of the data they were collecting and tracking for their veteran clients fit the definition of SDOH.
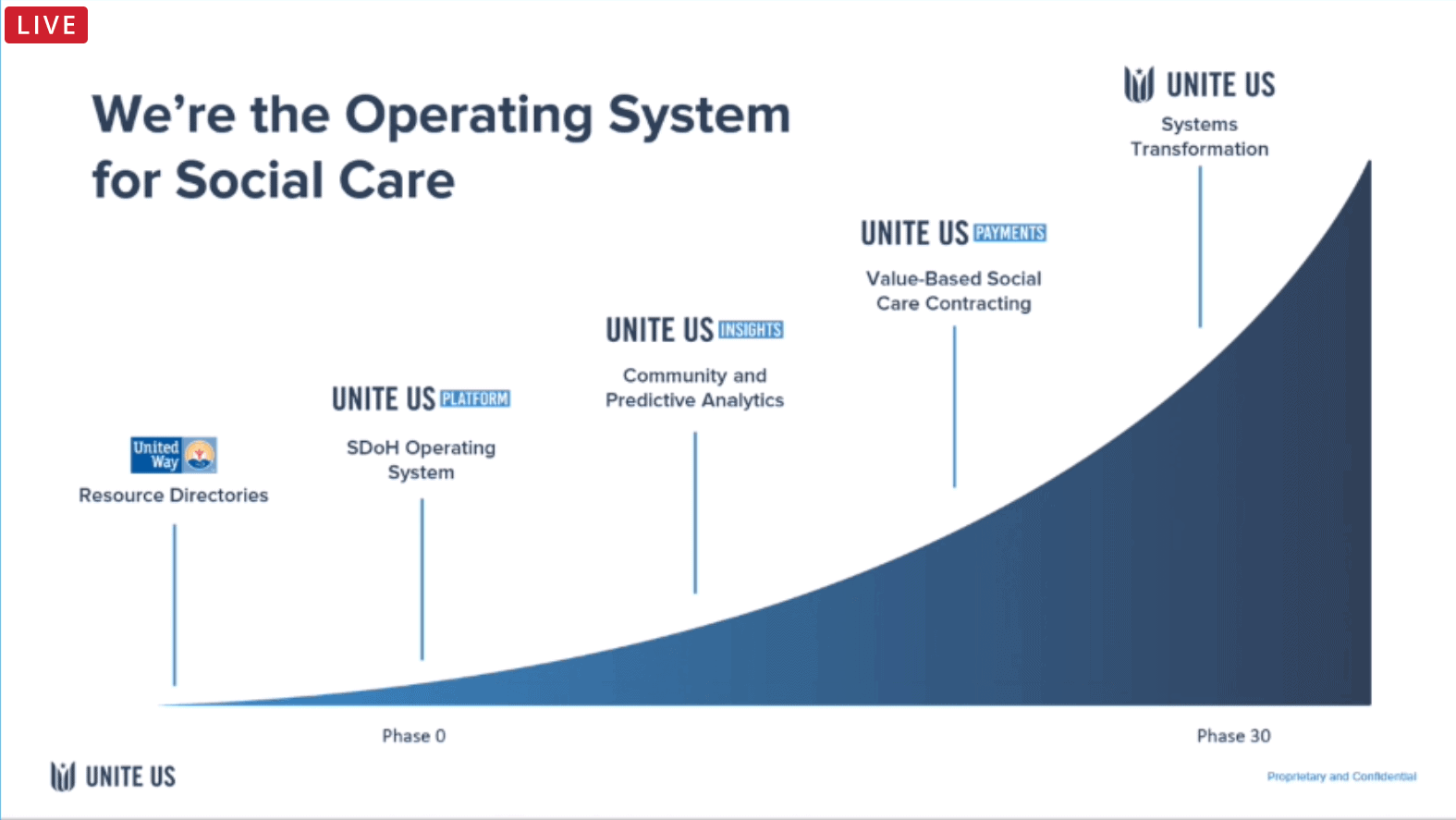
In 2013, Justice formed Unite Us to help communities do a better job of managing their resources for those who need them. In many communities, organizers use paper directories, phone services, and a collection of other tools to try and help those who need to find a resource. However, those systems are challenging. They force an individual to spend hours online looking up or calling resources to identify eligible services, whether they are accepting new patients or clients, and if they are close enough or offer hours of availability. Justice created Unite Us to automate as much of that process as possible and reduce the burden on both those seeking resources and the organizations or agencies providing the support services.
Justice noted that payers and providers are also quite interested in value-based social care contracting. It makes sense that if a clinician is trying to treat a patient’s asthma, issues in the home should be addressed at the same time, such as perhaps moldy carpeting.
As a platform, Unite Us is not positioned to replace existing systems like an EHR or an HIE. Instead, it is meant to augment and fill gaps, particularly on the community’s frontlines where social services organizations, non-profits, local agencies, and other stakeholders are found. The Unite Us platform provides a place for those organizations to connect, receive referrals, and share data, as appropriate. Referrals include the equivalent of Service Level Agreements (SLAs), so entities that participate in the Unite Us network are expected to respond quickly to any referrals they receive. There is no cost for community organizations to participate. However, they must agree to the SLAs, and they must agree to contribute outcome data to enhance the network’s value.
Unite Us’s approach is unique in that instead of launching a fixed solution and expecting every community and organization to conform, the Unite Us team goes into communities with a high-touch plan of engagement to determine the needs, opportunities, key resources, and Key Performance Indicators (KPIs) most relevant to a given community. It is a tailored approach to planning and engagement.
The company is currently working on major new projects in North Carolina to roll out services across all 100 counties (“NCCARE360”). The Nebraska HIE (NeHII) has also partnered with Unite Us to connect both clinical and social care networks to show more complete patient journeys.
In addition to the company’s care coordination services, Unite Us Insights provides data visualization services to view trends and population needs, including predictive capabilities that begin to identify patient needs and automatically assemble support packages for them based on available data. The company also now offers Unite Us Payments, a kind of “light” revenue cycle solution for services organizations.
As HIEs continue to source and incorporate SDOH, Justice reminded viewers that the community organizations (many of whom are fiercely protective of their patients) require direct and often person-to-person engagement. Relationship-building here is vital. Community and social care organizations are excellent sources of the SDOH data that HIEs and their members are looking for.
Creating Value through Collaboration: HIE-Payer Alliances at Work


- Date: Tuesday, September 8, 2020
- Presenters:
- Phil Beckett, CEO, Healthcare Access San Antonio (HASA)
- Dan Paoletti, CEO, Ohio Health Information Partnership
- Tracy Rico, Director Telehealth Services, Superior HealthPlan Centene
- Toria Thompson, Senior Program Manager for Integration and Interoperability, United Healthcare
- Moderator: John D’Amore, President & Chief Strategy Officer, Diameter Health
- Overview: Diameter Health and leaders from select HIEs and payers discussed examples of partnership opportunities that grow a network’s value, often led by payer priorities (such as HEDIS), along with some lessons learned.
The main theme of this session was the ongoing relationship-building between HIEs, payers, and, where needed, 3rd party vendors, to achieve specific goals. For example, as part of a collaboration, Superior HealthPlan Centene provided pharmacy claims data to HASA, which ED providers use to understand which patients are filling their prescriptions and whether they are filling them regularly. This information is of high-value to providers and the HIE brokering information between payers and providers. Superior can also see opportunities from this collaboration, such as patients who might qualify for a mail-order option because of limitations that make it difficult for them to fill their prescriptions in person.
On the payer side, the past five to eight years have been a learning experience, especially in terms of payers finding ways to accept, ingest, and use data that comes in newer formats. For example, payers are not always set up to accept CCDAs and, for their part, must go through processes of pairing data for ingestion where they have not needed to do so before. Their systems might be engineered to only accept claims data for HEDIS, incentive programs, and the like.
 The presenters zeroed in on the HEDIS reporting example and the potential challenges of HIE data in meeting NCQA requirements. Specifically, since HIE data could be overwhelming to trace through every point of origin, organizations might look to a certified intermediary as a partner.
The presenters zeroed in on the HEDIS reporting example and the potential challenges of HIE data in meeting NCQA requirements. Specifically, since HIE data could be overwhelming to trace through every point of origin, organizations might look to a certified intermediary as a partner.
NCQA did not recognize a CCDA as certified, and the teams involved in the Ohio partnership needed to ensure that only certified source data was passing through to United Healthcare. The system had to convert QRDA I data, output as a CCDA with only certified data elements, and then process it as a pseudo-claim. In the example provided, Diameter Health was already NCQA certified for a number of measures. By pushing HIE data through Diameter Health, all parties were able to meet NCQA requirements.
After going through all of these steps, the HIE, NCQA, Diameter Health, and United built trust and understanding in both this process and, consequently, the data. NCQA auditors can each look for different things, and it took relationship-building and a commitment to finding innovative solutions to get through the challenging steps.
Dan Paoletti pointed out that data governance is essential, including engaging partners to define what is most important to them. In discussions with payers, the importance of HEDIS and care coordination for high-risk patients came out on top. To support the payer’s needs, an HIE thus had to develop the data to support those measures and related insights.
Phil Beckett offered that some of the biggest challenges his team saw in their payer collaborations were understanding how payers needed to receive and use their data, and then go back to the sources to resolve data gaps or quality issues. He credited Diameter Health with helping to identify data improvement opportunities.
The Q&A section focused on validation and data quality. A few highlights:
- The U.S. Core Data Set for Interoperability (USCDI) requires authentication and signatures, which will help expand use cases to risk adjustment and others.
- The Data Aggregator Validation program from NCQA will bring additional rigor for HIEs in 2021. There is currently a pilot underway.
- NCQA auditors have focused on a chain of custody to ensure no changes were made to data along the way. With aggregators like HIEs, this changes by the nature of aggregation. Companies like Diameter Health improve data quality with standards such as codes, but there is still a need to convince auditors that these “improvements” do not change or affect the nature of the original data.
Enforcement of the Information Blocking Rules is Coming (Soon!) – Is Your HIE Ready?

- Date: Tuesday, September 8, 2020
- Presenters:
- Deven McGraw, Chief Regulatory Officer, Ciitizen
- Amy Warner, General Counsel, Privacy and Compliance Officer, Rochester RHIO
- Overview: Deven McGraw and Amy Warner provided a summary of the Information Blocking Final Rule and its implications for HIEs over the next year.
McGraw and Warner opened with a review of definitions. Electronic Health Information (EHI) is data that meets the HIPAA definition of “designated record set.” Organizations that exchange EHI only for research purposes are not defined as an “Actor” (covered by the rules). However, any organization meeting the other basic criteria and sharing data for treatment, payment, or operations would qualify as an Actor and would be subject to the new rules. Data blocking is not limited to preventing or impeding individuals from accessing their information. However, the rule only applies to EHI; paper records are not covered.
The final rule was published on May 1, 2020, but does not go into effect until November 2, 2020. At some point after that, the HHS Office of Inspector General has the authority to begin investigating and potentially issuing penalties of up to $1 million per violation.
McGraw and Warner listed the following examples of potential information blocking violations:
- Restricting access, exchange, or use of EHI that is authorized under applicable state or federal law for treatment and other permitted purposes.
- Implementing health IT in nonstandard ways that are likely to substantially increase the complexity/burden of accessing, exchanging, or using EHI.
- Implementing IT in ways that could restrict access, exchange, or use of EHI with respect to exporting complete information sets or facilitating transitions between health IT systems.
- Implementing IT in ways likely to lead to fraud, waste, abuse, or impede innovations or advancements in EHI access, exchange, or use.
The goals of the rule are to remove barriers to exchange and encourage patients to access and use their own information; ensure health care professions, payers, and providers, have access to data to provide care and improve quality and population health management; and to support public health and safety, such as in public health emergency response efforts.
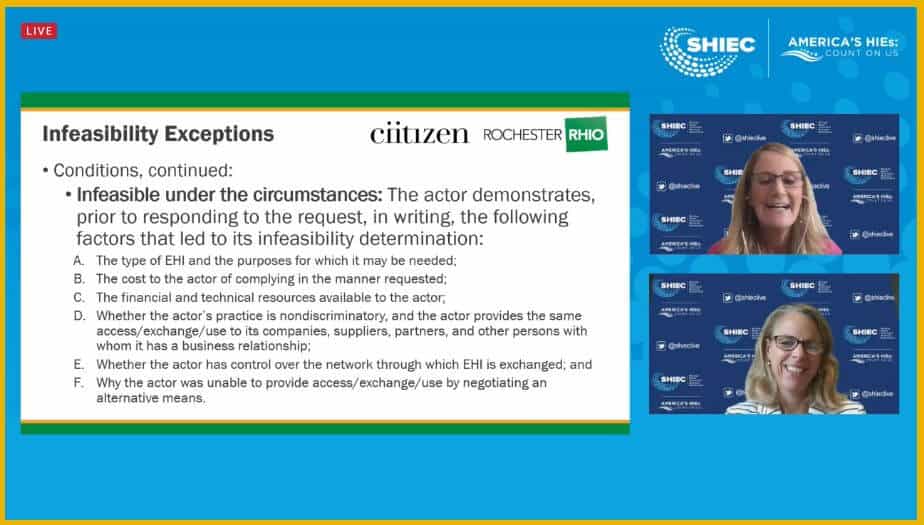 The presenters described the eight exceptions for information blocking that HIEs should become familiar with. They discussed that while patient portals are not specifically required as a way of responding to information requests from patients, the rule intends to make sure HIEs are not looking for ways to drag their feet and avoid having to respond to such requests. HIEs will need to think about how they can provide alternative mechanisms to respond to individual patients’ requests for their information, in addition to ensuring there are no (unnecessary) blocking practices, policies, or technologies in place that slow or prevent information moving between HIE partners who are otherwise entitled to access that data for treatment, payment, and operations.
The presenters described the eight exceptions for information blocking that HIEs should become familiar with. They discussed that while patient portals are not specifically required as a way of responding to information requests from patients, the rule intends to make sure HIEs are not looking for ways to drag their feet and avoid having to respond to such requests. HIEs will need to think about how they can provide alternative mechanisms to respond to individual patients’ requests for their information, in addition to ensuring there are no (unnecessary) blocking practices, policies, or technologies in place that slow or prevent information moving between HIE partners who are otherwise entitled to access that data for treatment, payment, and operations.
A careful review of existing data-sharing agreements and Business Associate Agreements (BAAs) is highly recommended to ensure an HIE does not have language in place that runs counter to the final rule.
Patient Centered Data Home™ (PCDH)
- Date: Thursday, September 10, 2020
- Presenters:
- Angie Bass, CEO, Midwest Health Connection
- Brandon Neiswender, Vice President & COO, Chesapeake Regional Information System for our Patients (CRISP)
- Moderator: Keith Kelley, COO, Indiana Health Information Exchange (IHIE)
- Overview: Keith Kelley (Indiana Health Information Exchange), Angie Bass (Midwest Health Connection), and Brandon Neiswender (Chesapeake Regional Information System for our Patients) discussed the current work of the Patient Centered Data Home initiative, next steps, and the PCDH’s position in the national HIE landscape.
The Patient Centered Data Home model is built on the idea of enabling the faster exchange of patient information when patients leave their “home” HIE. This departure could be for travel, relocation, or simply work commute reasons. When a patient departs from their home HIE and has an encounter with the healthcare system, the PCDH becomes the conduit to move the patient’s information for that specific episode of care back to their home HIE to notify care team members.
The federal government has begun to show interest in this model. PCDH supplements existing message and notification activity among HIEs with over 16 million transactions per year.
PCDH supporters recognized a need to conduct a more thorough business strategy assessment, so they created the Business Strategy Workgroup. Angie Bass chairs that committee and presented information on specific steps they took to define a sustainable future for PCDH.
Bass’s team started with a governance assessment. They recognized the current national-level collaborative effort with early adopters and supporters but also understood that a friendly partnership with a handshake or two would not be sufficient to sustain PCDH into the future. For this reason, one of the work group’s recommendations is for PCDH to pursue a legal structure with its own governance, policies, and agreements for data sharing. The intent is to form a 501(c)3 not-for-profit corporation while still providing a collaborative place for everyone to participate and gain value, depending on what they are able to do based on their own states’ laws and limitations.
The group also looked at technology and worked on a roadmap to consolidate services and technology acquisition. In addition, Bass’s team discussed an overall business model that might make sense for PCDH. It is clear that sustainability is a basic requirement, so funding is the most important aspect to consider. The workgroup has partnered with a consulting firm to assist with this specific assessment and plan.
Keith Kelley listed four expectations/priorities for PCDH. It:
- Must expand and ensure that the original mission is met (i.e., ensure providers have access to patient data wherever it was created).
- Ensure data sharing standards
- Create deeper collaboration between HIEs
- Innovate on business models
Kelley explained that it is important to not only think about PCDH in terms of faraway places (traveling) but also to think about cross-border sharing closer to home, such as where people live near state borders and commute between states for work.
Brandon Neiswender spoke about CRISP’s collaboration with neighbors, which has positioned all parties in CRISP’s region to better serve stakeholders.
 The presenters believed that PCDH could serve a role in defining standards for data sharing. In addition, there are ongoing conversations to help determine PCDH’s role in the national landscape vis-a-vis eHealth Exchange, Carequality, CommonWell Health Alliance, and TEFCA as it continues to take shape.
The presenters believed that PCDH could serve a role in defining standards for data sharing. In addition, there are ongoing conversations to help determine PCDH’s role in the national landscape vis-a-vis eHealth Exchange, Carequality, CommonWell Health Alliance, and TEFCA as it continues to take shape.
The key need at the moment is to actively engage in more discussion. The panelists believe that healthy conversation will innovative business models, define relationships between PCDH and other national networks, and establish the value proposition in how PCDH is viewed as an essential component of the national ecosystem of patient information exchange.
HIE members should expect to contribute financially in the beginning. Member fees will not be the long-term strategy for sustainability, however. While these fees might be a near-term feature, panelists discussed the need to provide value back. Decisions have not been finalized, but PCDH might also look at facilitating new revenue opportunities for participating members.
Panelists responded to a number of questions, including one about whether for-profit members would be allowed to participate. Generally, the sentiment was that PCDH would need to find ways to include vendors and for-profit partners, despite the history of HIEs having concerns about unintended data use (that they are responsible for) or potential competition. Bass felt it was important to make it known that HIEs have put in a lot of time, money, and effort to build what exists today, and they will have to find suitable ways to partner and prevent one party from profiting from the hard work of others.
The group also discussed potential changes to definitions of triggering conditions for notifications across PCDH. Today, differences in Zip Codes can be used as a trigger, and the group felt that this notification probably wouldn’t work for other participants beyond HIEs in the future. Work will need to be done to define new criteria.
While PCDH leaders continue to work through the details of what comes next for PCDH, aside from the next most immediate step (which is to set up a legal structure), Kelley advised viewers not to sit on the sidelines until the details are all worked out. Instead, PCDH encourages viewers to join the conversation to influence its direction and the decisions that are made in the coming months. For anyone interested in learning more about PCDH involvement, please contact Melissa Kotrys, the current chair of PCDH at SHIEC.
Roads, Ramps and Parking Lots: Health Current’s Roadmap for Future Success (2020 to 2022)

- Date: Thursday, September 10, 2020
- Presenters:
- Melissa Kotrys, CEO, Health Current
- Christy Dye, Chief Business Development Officer, Health Current
- Overview: Melissa Kotrys and Christy Dye from Health Current walked viewers through their 2019/2020 strategic plan and what effects the COVID-19 pandemic had on modifications to that plan.
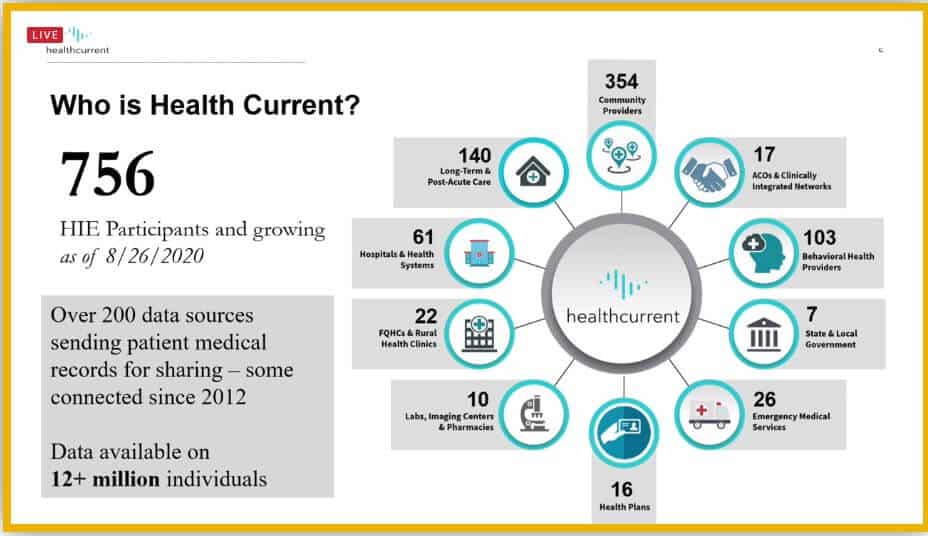
Health Current is an HIE serving the state of Arizona. Melissa Kotrys, CEO of the organization, began the session by providing an overview of the HIE and its operating activities.
In 2020, Health Current has processed 96% of the inpatient discharges and 99% of the Emergency Department visits across Arizona. Health Current supports more than 13 million patients and processes 23 million transactions per month over connected 200 data sources.
 This past year, Health Current’s leadership began a strategic plan update for the next three years. They started by gathering input from thirty-six stakeholder interviews (each interview 90 minutes) from healthcare leaders across the state, conducting a participant satisfaction survey (2019), holding an annual user group meeting (2019), and facilitating ongoing conversations with board members and community stakeholders.
This past year, Health Current’s leadership began a strategic plan update for the next three years. They started by gathering input from thirty-six stakeholder interviews (each interview 90 minutes) from healthcare leaders across the state, conducting a participant satisfaction survey (2019), holding an annual user group meeting (2019), and facilitating ongoing conversations with board members and community stakeholders.
Health Current focused heavily on Social Determinants of Health (SDOH) and Advance Directives in this first year of its 2020-2022 strategic plan. In the previous year (the last year of their 2017-2019 strategic plan), Health Current focused on public health initiatives.
One fundamental shift worth noting between the ‘17-’19 and the ‘20-’22 plan is an understanding that an HIE’s true foundation is not merely aggregating and sharing data, but combining data, technology, and trust.
Health Current had eight essential success factors:
- Gather data; more data is essential to an HIE’s value
- Associate data from different sources in meaningful ways to support the community
- Promote complete, consistent, and coded data to be useful and trusted
- Deliver data customized to the various ways that stakeholders feel able to use it (care coordination, quality improvement, predictive modeling, etc.)
- Focus on innovative opportunities to promote Arizona as a top healthcare community
- Support the community as the ideal organization to implement statewide tools and initiatives
- Seize opportunities to lead in the national interoperability space to benefit Arizona
- Always monitor long-term sustainability
Kotrys described Health Current’s approach to organizing the potential areas of focus for their updated strategic plan. The basic approach was to categorize initiatives and projects based on whether they were already being worked on (On the Road), were close to being started but needed additional planning (On the Ramp), or were not yet well-defined or urgent enough for either of those categories (Parking Lot).
The Health Current team evaluated projects for major areas of interest and placed them into the Road, Ramp, or Parking Lot category. These interest areas included adding new data types to fill gaps, creating real-time alerts, and implementing care coordination, interoperability, and infrastructure projects. This organization helped the team stay focused and develop reasonable timelines for the remaining work.
Some sample projects include Medicaid’s focus on SDOH, which has been in planning for the past few years, a robust consent management portal, an opioid treatment registry (live this summer), and bi-directional connectivity with the state’s immunizations registry.
Christy Dye joined Health Current in February 2020 as Chief Business Development Officer and was charged with carrying out the new strategic plan. Three weeks later, COVID-19 was on the radar. One of the critical lessons Dye learned during that time was to “keep moving, get creative, and be flexible.”
Dye presented four domains that required special attention during the COVID-19 response. These were:
- Communication strategy
- Marketing strategy
- Training strategy
- New product/service development
Each was directly affected by COVID-19 and was carried out with COVID-19 as the major driving force in Spring 2020. For example, the communication strategy quickly became “COVID-flavored” and included the following:
- Regular email notices on new COVID-19 lab test alerts service
- FAQs
- Medicaid MCO Web page
- Campaigns targeting new HIE participants, especially labs, behavioral health providers, and skilled nursing facilities
- Campaigns educating existing participants on new COVID-19 cases and trends
Over the summer, the Health Current team also worked through streamlining product development from idea generation through roll-out to more quickly respond to needs and opportunities across the state.
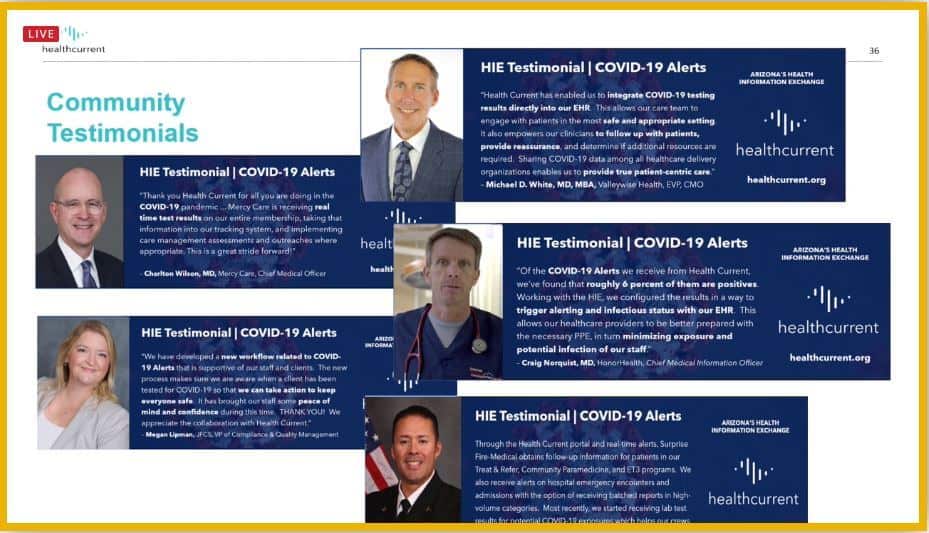 In addition to its internal initiatives, Health Current supported the Arizona Department of Public Health by providing HIE portal access for case investigators, syndromic surveillance, data extracts and weekly reports on COVID-19 positive patients, real-time data from hospitals about bed capacity and other key metrics, and alerts for COVID-19 positive lab results.
In addition to its internal initiatives, Health Current supported the Arizona Department of Public Health by providing HIE portal access for case investigators, syndromic surveillance, data extracts and weekly reports on COVID-19 positive patients, real-time data from hospitals about bed capacity and other key metrics, and alerts for COVID-19 positive lab results.
Kotrys and Dye are making plans to extend their planning capabilities in future years based on their pandemic experience this year. Such capabilities include building in agility and flexibility, creating rapid response pathways to answer questions and meet needs from partners, and conducting proactive data quality work to ensure that it is ready when needed.
The presenters were asked whether Health Current is planning to participate in the TEFCA/QHIN model. Health Current is currently monitoring the developments of TEFCA and QHINs and will evaluate whether participation is right for Arizona when more details are available.
How Can HIEs Supercharge Data Research to Change Medicine?
- Date: Thursday, September 10, 2020
- Presenters:
- Marc Horowitz, Business Development Executive, Clinithink
- Salim Kizaraly, SVP Business Development, Stella Technology
- Drew McNichol, Chief Technology Officer, HEALTHeLINK
- Overview: Leaders from HEALTHeLINK, Clinithink, and Stella Technology talked about a project that uses data to identify patients at risk for developing Non-Alcoholic Fatty Liver Disease (NAFLD) and the success they had in affecting clinical care.
Drew McNichol, CTO at HEALTHeLINK, discussed the purpose of their grant-funded research project and some of its history. The research goal was to determine whether the unstructured narrative in clinical documents could be used to improve the identification of patients at risk for NAFLD. HEALTHeLINK partnered with a leading provider in Liver Disease who believed that certain patient traits could be used to predict NAFLD in at-risk patients.
Investigators used a combination of structured data (specific scores and diagnoses) and unstructured data (steatosis of the liver without alcohol, NASH or cirrhosis focused on non-alcoholic steatohepatitis, patients with liver ultrasound or liver CT scan, diabetes diagnosis, BMI, and other factors contained in the narrative) to develop risk profiles.
The team began by loading structured data into Stella Technology’s Prism solution, which analyzes, cleans, and prepares data. Prism then assigns data to categories (similar to FHIR resources) that analysts can use more easily when working with the scrubbed data.
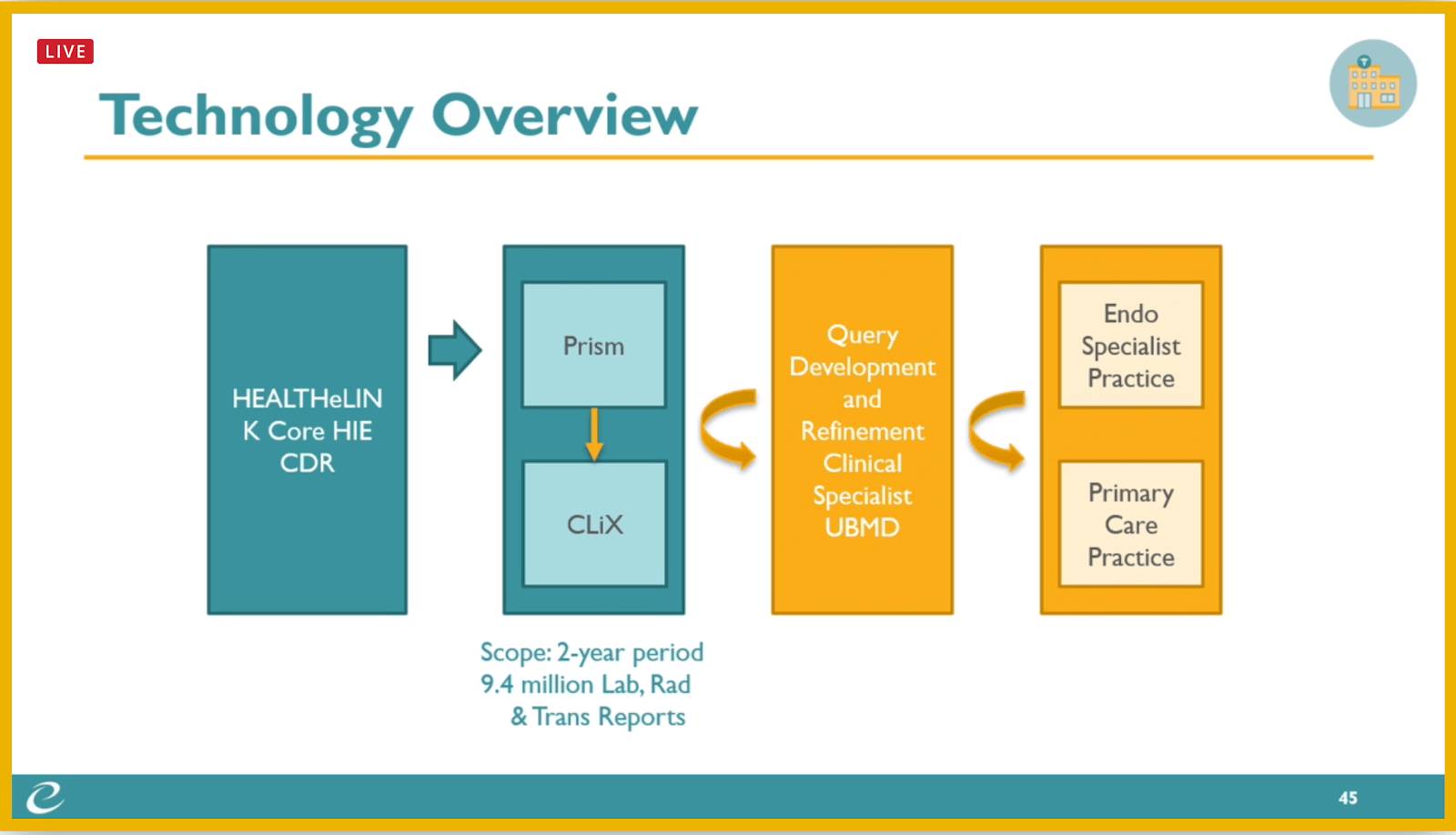
For the unstructured data, HEALTHeLINK used Clinithink’s CLiX solution using Natural Language Processing (NLP) to “read” narrative sections of clinical documents. This solution can confirm what exists in the structured data and also spot differences that might be important. For example, while a patient might have no known allergies in the structured data, the narrative may mention a family history of certain allergies that other clinicians should know about.
Results for the structured data showed over 2,300 patients at risk for NAFLD, and approximately 50 additional patients were identified from unstructured data analysis. Due to time constraints for the grant, researchers selected the top 50 results from the combined set. Of the 50 selected, 46 had risk factors for NAFLD that would otherwise have been missed.
Data was ultimately adjusted since some structured data included heavy alcohol users in the original population.
The team then shared their initial results with practices to give to clinicians for feedback. They were met with very positive reactions. In one case, a provider said, “this is what we’ve been waiting for HEALTHeLINK to do!”
Presenters offered the following observations from their research project:
- Availability of an open, flexible Clinical Data Lake allowed for iterative data/query requirements and quick project turnaround
- Free text narrative is indeed valuable in identifying additional at-risk patients missed if using structured data only
- There is value in identifying false positives, i.e., exclude patients with alcohol usage recorded in text
- A limitation is that PDF documents were excluded; there is additional work involved in making data in such files available for this type of study
- Sufficient time is needed to develop, refine, and validate queries
The presenters believe that there is absolutely value to be found in unstructured data. The team is continuing their work today to refine and expand to additional practices and are looking at applying these solutions to other diseases such as diabetes.
The team felt that it has been difficult to use unstructured data in the past because the tools were insufficient. As technology improves and as demands increase to conduct more analyses quickly and across larger geographies, there will be significant opportunities for HIEs to become involved in this type of work. This involvement could range from participating in clinical trials (appropriate populations must be identified even before a clinical trial begins), monetizing de-identified data, and partnering with companies like pharmaceuticals or payers to provide data analysis or high-risk population monitoring solutions. HIEs can also bring additional types of data to bear that others might not have access to. For example, HIEs with access to extensive SDOH data can bring that data into analysis, such as for NAFLD risk assessments.
Overall, the team recommends starting small with these types of research projects, identifying a physician champion, setting up a research sub-committee, and partnering with research institutions to provide guidance and resources for IRB compliance.
| Week One Summary | Week Two Summary | Week Three Summary | Week Five Summary |
|---|
Thank you for joining us this week at SHIEC. Stay tuned for week five’s recap!
J2 Interactive is an award-winning software development and IT consulting firm with a specialty in customized solutions for HIEs. Read about HIE platform migration.
We would be happy to have a no-obligation discussion about your HIE’s needs with you.



