| Week One Summary | Week Two Summary | Week Three Summary | Week Four Summary |
|---|

2020 marks the sixth year of SHIEC and the first year of it going virtual! Join us over the next five weeks from August 17 – September 15 as we recap the 10-day series of virtual sessions!
Building a Thriving HIE Model: Perspectives from 3 HIEs
- Date: Tuesday, September 15, 2020
- Presenters:
- Hans Kastensmith, Executive Director, Idaho Health Data Exchange
- Larra Petersen-Lukenda, Chief, Population Health, Nebraska Health Information Initiative
- Steve Rottmann, COO, Wisconsin Statewide Health Information Network (WISHIN)
- Vineeth Yeddula, CEO, KPI Ninja
- Overview: Leaders from Nebraska Health Information Initiative (NeHII), Idaho Health Data Exchange (IDHE), and Wisconsin Health Information Network (WISHIN) discussed their roles in statewide HIEs, their initiatives to serve their members and seek financial sustainability, and their plans for the future.
The convergence of HIEs reaching financial sustainability through diversified sources of revenue, improved standards and efficiencies (associated with moving data to where it is needed), growing data needs (stemming from pay for performance programs), and increasing demand (for using data to understand new and growing numbers of use cases in healthcare) have positioned HIEs for growth. It has also anchored themselves in decision-makers’ minds as essential resources and candidates for a single source of truth.
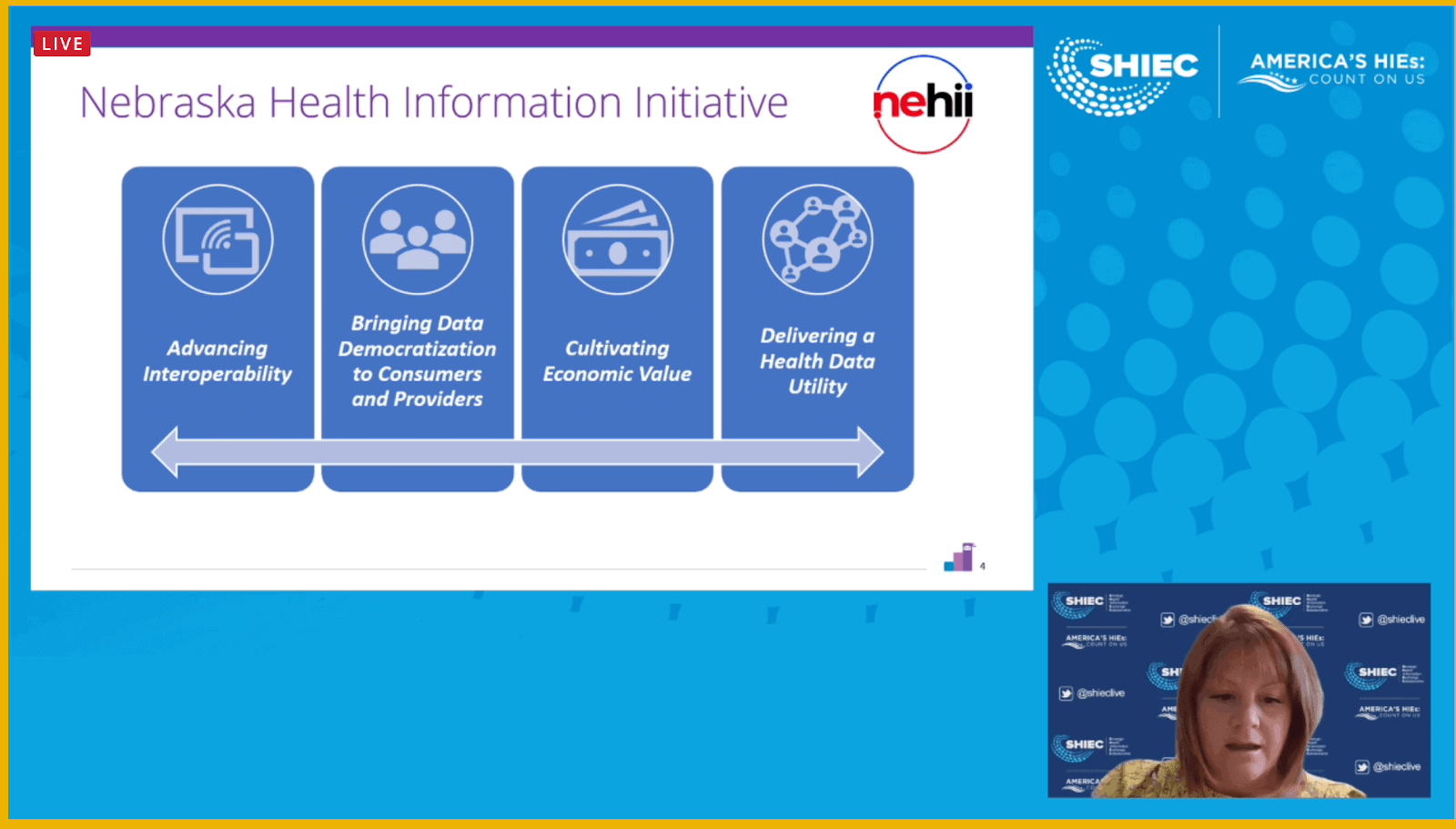
Larra Petersen-Lukenda opened the session by providing an overview of NeHII’s approach to optimizing the value of data for its stakeholders. Specifically, Petersen-Lukenda discussed treating their HIE and its assets as a health data utility and aligning HIE activities and programs with public goals. NeHII prioritizes removing barriers to put the right kind (and right amount) of data in the right places for optimal effect. For example, clinicians will often need to see data from a patient’s record that the patient might not be as interested in seeing, and vice versa.
NeHII has been modeling its future as a health data utility aligned with public goals. Today, NeHII focuses on four values:
- Advancing interoperability
- Bringing data democratization to consumers and providers
- Cultivating economic value
- Delivering a health data utility
Projects are reviewed with these values in mind before they are initiated. Examples of projects that fit well with these stated values include:
- Syndromic surveillance, electronic lab reporting, COVID-19 reporting, and data governance (focused on what data to share with whom and how best to inform stakeholders about acceptable use) in partnership with Medicaid and state public health departments.
- Quality payment programs, value-based care, eCQM/quality measures, and measurement and reporting for health systems, providers, and payers to reduce the reporting burden on stakeholders.
- Social determinants of health platform, QCDR/measure development, Gravity Project, and NQF partnership with CMS, ONC, and the CDC.
As NeHII has adapted over the last several years, leadership saw a need to carve out specific resources for certain stakeholders to deliver what was needed. To provide these resources, NeHII spun off different entities focused on different types of work.
NeHII’s core is still the HIE and related operations. These operations include PDMP, SDOH, Electronic Lab Reporting, Syndromic Surveillance, consent management, hospital/provider onboarding, patient portal, etc.
For their academic and research interests, NeHII created the Nebraska Healthcare Collaborative. This group focuses on grants, health data science training, handling new research requests, and other aspects of maintaining relationships with academic institutions across the state.
NeHII also saw a need for consulting services, and to respond to it, the HIE created NeHII Shared Services. This entity supports applications used for care management, event notification services, analytics consulting, dashboard design, quality reporting, predictive modeling, data extraction and engineering, workflow integration, program/project management, and data governance consulting.
The final spin-off entity is the NeHII Foundation, which focuses on community engagement and philanthropy, donations, project investment, endowed chair, and university contracts.
Hans Kastensmith presented an overview of the “super stack” of solutions that Idaho Health Data Exchange assembled to respond to Idaho’s identified needs. Kastensmith described an environment where supporting ACOs was important, as was reaching a sizable rural population. IDHE noted that many rural providers were unable to acquire the technologies and levels of sophistication necessary to deliver or use the services that HIEs provide. In looking for funding to help subsidize efforts to support rural providers, IDHE identified the need to support payers with HEDIS. This type of support was new for IDHE, but they developed a strategy to move in this direction.
IDHE also felt that while the standard connections with hospitals and provider offices were necessary, major portions of care from post-acute and community organizations were still being missed. IDHE needed to find ways to add to their network to fill gaps.
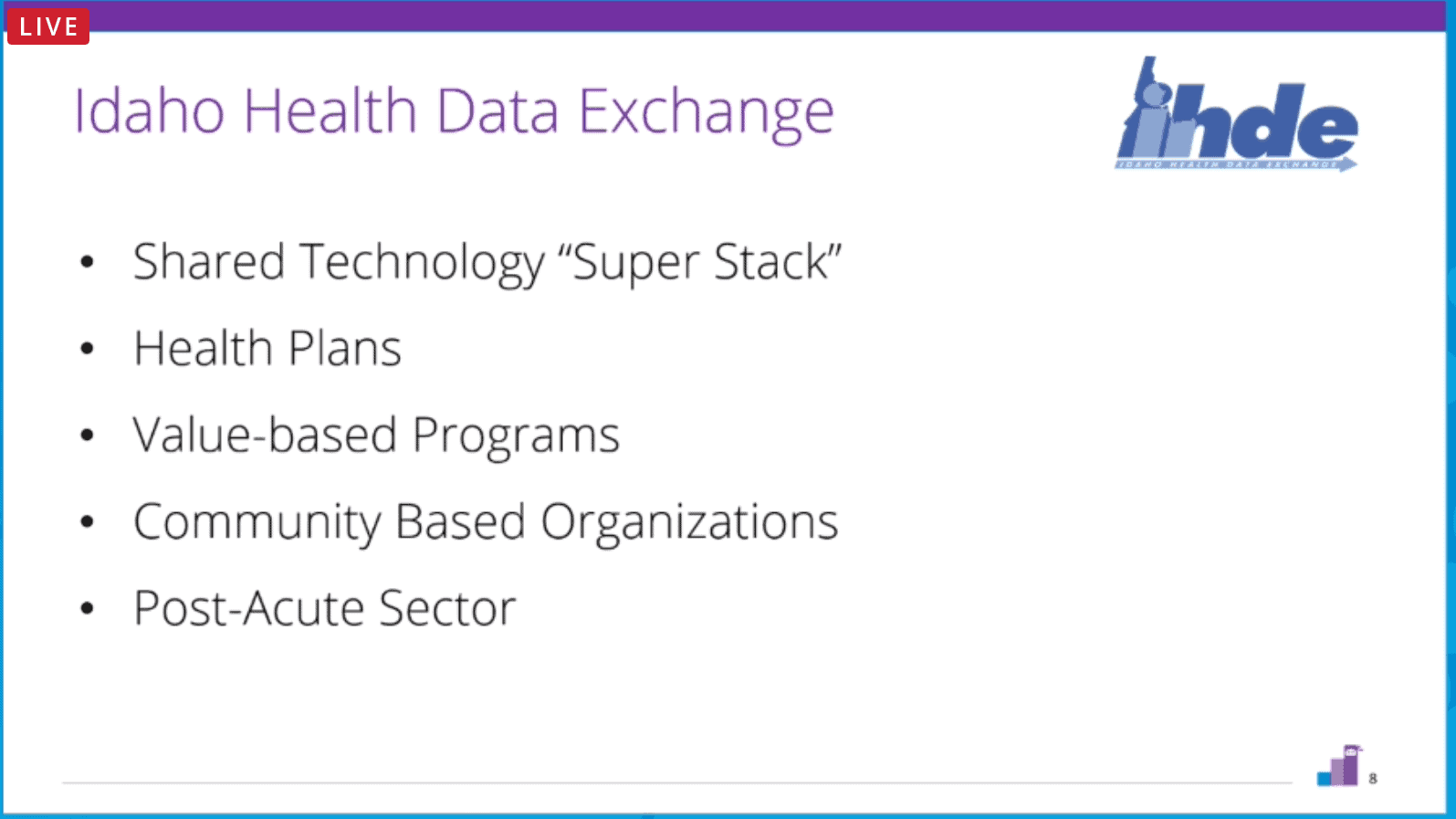
Kastensmith discussed the importance of data quality and the fact that it was a major concern at IDHE. Leadership at IDHE contracted with 4medica to assist in cleaning up identity matching and remove thousands of duplicates. Now, IDHE has less than a 1% duplicate rate.
IDHE then contracted with TermAtlas to codify data where possible and make more of IDHE’s data machine-readable. The team at IDHE invested in building their own version of an EDW that they call “Lake on FHIR.” It is a FHIR-based data warehouse that makes data resources relational. IDHE is now able to keep pace with advances in HIE practices as FHIR becomes more mainstream. This platform allows IDHE to add new FHIR resources at any time and re-populate their EDW within a few days as new data types become available. IDHE then partnered with KPI Ninja to develop an advanced analytics program leveraging a wider side of IDHE’s data.
IDHE also partnered with myhELO to support smaller practices in leveraging telehealth to respond to the concern that rural practices had difficulty acquiring this type of technology. The HIE took on the burden of standing up the technology and making it available to those practices across the state. IDHE then partnered with UHIN for cross-border alerts as patients moved between the states.
In addition, IDHE partnered with Aunt Bertha (known as the “Social Care Network”) to engage the community-based organizations that IDHE sought to include in the state’s broader network. Aunt Bertha essentially provides a Social Determinants of Health platform, and users can access it through Single Sign-On from IDHE. Aunt Bertha offers assessment tools and then displays resources based on the outcome of the assessment. It also enables closed-loop referrals and follow-up.
ConnectAmerica was the last part of what IDHE called its “Super Stack” of solutions. IDHE identified a need to treat patients at home. As COVID-19 emerged, visits moved to virtual visits, but virtual monitoring was still not fully supported. There were often barriers for individual practices to contract and integrate with remote monitoring services to get monitoring data back into their EMRs. The partnership with ConnectAmerica allowed IDHE to offer smaller practices that had existing integration with IDHE an opportunity to add remote monitoring with no additional investment other than ordering the technology used by patients in the home. IDHE’s “Super Stack” has helped to accelerate the organization’s ability to respond to key needs across the state and deliver value in the eyes of its broad base of diverse stakeholders.
IDHE continues to move toward greater funding self-sufficiency with less reliance upon grants. As with other HIEs across the country, part of the strategy to achieve that financial independence includes focusing on payer and public health partnerships where the HIE can relieve reporting burden, bridge unique data gaps, and be valuable to a number of initiatives, such as Learning Health Networks across the state.
This session’s final segment was a presentation from Steve Rottmann at WISHIN, which serves more than 7 million patients as the state-designated HIE in Wisconsin. WISHIN supports approximately 1,800 care sites, including PCP offices, post-acute facilities, health plans, MCOs, hospitals, correctional facilities, and community organizations.
Rottmann discussed how data can be overwhelming for PCPs and smaller organizations. WISHIN’s strategy has been to work with EHR vendors to integrate a single hub to accelerate onboarding and participation among smaller practices and organizations. The HIE is in a position to connect a wide variety of services, including routing alerts and information between EMS providers and hospitals.
The concept of pushing information is central to WISHIN’s strategy. Wisconsin’s municipalities have their own health departments, and there are opportunities to help make those local departments aware of various cases or conditions where the health department might need to respond quickly to do a follow-up. WISHIN’s goal is to push information immediately and avoid days of delay from traditional information sharing practices.
Like many other HIEs today, WISHIN is actively engaged in conversations with stakeholders to identify data and service gaps where the HIE can provide value. This engagement is an important change from just a few years ago. Rottmann recalled experiences from early 2018 when HIE services were becoming available, and one of the first comments he heard was, “What can I use the data for?” That has changed, and many more stakeholders have a better understanding of the value of HIE data and have specific questions to ask of that data.
WISHIN is moving towards supporting HEDIS requirements with a group of payers and auditors, working through a proof of concept for the HIE to meet both supplemental and non-supplemental data requirements.
Rottmann provided one example of the kinds of projects WISHIN is undertaking today. In Milwaukee, thousands of individuals use Emergency Departments as their primary care. As these patients arrive, WISHIN makes physical, behavioral, and social health needs data available so that a trained resource can be dispatched while the patient is still in the Emergency Department. This resource then retrains the patient and guides them to use resources in the community other than the Emergency Department.
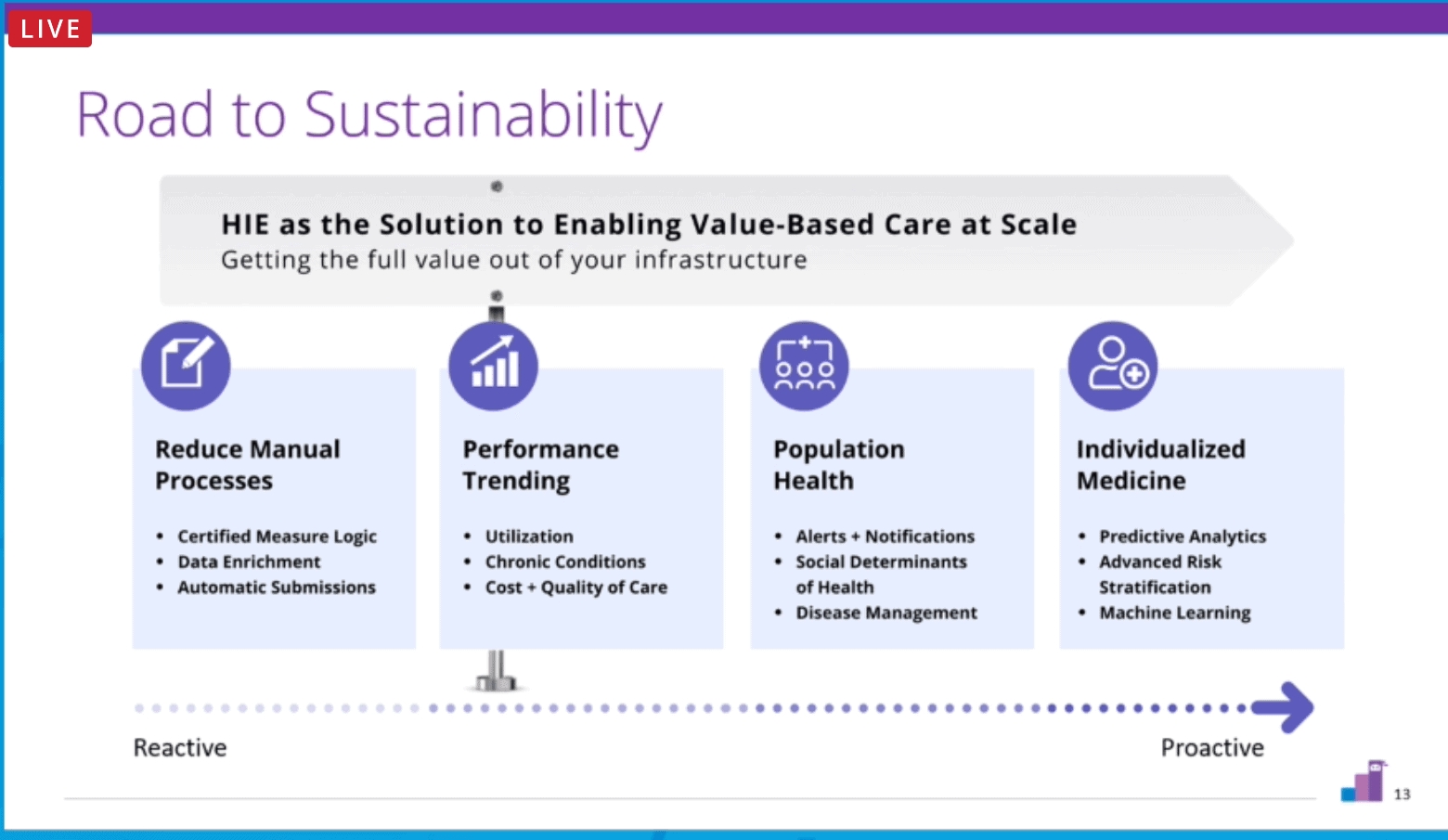
KPI Ninja’s Vineeth Yeddula wrapped up the session with a few observations:
- There is renewed interest among HIEs in public health partnership and much stronger alignment with CMS, ONC, and NCQA and their initiatives.
- HIEs are quickly moving beyond clinical data to provide a greater variety of unique data (and value) for their stakeholders.
- There is a major focus on pushing data out to stakeholders rather than HIEs waiting for stakeholders to query or request information.
- It is increasingly important for HIEs to align with payment programs, both government-funded and privately funded.
As HIEs move from reducing manual burden to providing: monitoring and trending, population health analytics and alerting, individualized medicine in the form of advanced risk stratification, predictive analytics, and machine learning and AI, it is essential for HIEs to remember to listen carefully to their member organizations. As soon as a need is presented, the HIE should focus time, energy, and resources on delivering what is needed. Responding in this way—one request at a time—is how HIEs are rapidly building credibility, referrals, and models for financial sustainability.
More Than Attestation: Promoting Interoperability at the Point of Care

- Date: Tuesday, September 15, 2020
- Presenter: Rhonda Spellmeier, HIE Workflow Specialist, KONZA
- Overview: Rhonda Spellmeier described her role as KHIN’s workflow integration specialist, what she does in that position, and the role’s value for both the HIE and its member organizations.
KHIN operates as a regional subsidiary of KONZA and is based in Topeka, Kansas. The HIE offers a variety of services ranging from traditional HIE message and data transaction services to real-time alerts, analytics dashboards, messaging, QCDR, and public health reporting.
Rhonda Spellmeier, HIE Workflow Specialist for KHIN, described the work she does on behalf of KHIN’s stakeholders. In her role, there is a heavy emphasis on work done at the point of care. In essence, she is responsible for engaging with stakeholder organizations like hospitals or practices, especially at the department level, and evaluating and consulting with administrators, staff, and clinicians to optimize workflows with available data and best practices.

The workflow specialist position originated from a KONZA strategy to bridge the gap between technology and clinicians at customer sites with a technically proficient clinician provided by the HIE. KHIN recognized that many organizations had access to data, but organizations were not necessarily making full use of that data or using it in all of the ways they could.
Responsibilities of the workflow specialist include:
- Assisting healthcare providers with the development of a process map that identifies how health information is shared between disparate providers, including the current health information exchange process.
- Assisting healthcare providers in developing a linear workflow plan that creates new workflow patterns to bolster the use of health information exchange, data sharing, and population health tools.
- Identifying barriers in other healthcare facilities that affect the use of health information exchange and population health tools.
- Identifying strategies for reducing barriers to the use of health information exchange at the facility.
- Effectively communicating strategies with healthcare providers and leadership at participating organizations.
- Regularly monitoring health information exchange and population health tool usage at member sites.
- Assisting providers and their staff in the development of ongoing training plans to ensure new staff understands the workflows.
- Providing ongoing training, as needed, through in-person meetings, webinars, and other training tools.
- Conducting regular travel on-site to implement provider and staff usage plans and strategies for the HIE’s tools and services.
Spellmeier described the value of equipping herself with as much information as possible from public information sources and staff usage statistics before engaging with client leadership, using that information as part of the workflow specialist’s consultation process. She employs a structured approach to conducting her assessments, much like performing a patient assessment. The assessments’ results help identify sites or departments that would benefit from optimization efforts, and the workflow specialist then initiates contact with those member organizations.
Sometimes consultative engagements are short and require only supplemental training. In other cases, much more extensive workflow modifications are recommended and supported by leadership, resulting in engagements that can last for more than a year.
Spellmeier offered the following insights that help to create a successful workflow specialist program at an HIE:
- Get early buy-in from executive leadership and stakeholders. Department leadership buy-in is essential; department heads are typically the ones leading change within a department. These might be an HIM Director, lead pharmacist, nurse manager, etc.
- Engage at least one clinical champion. They are often quite busy, but once engaged in the project, they can be an internal resource, serve as a superuser, and can help remove barriers to implementing workflow changes.
- Identify priority areas for engagement and where the workflow specialist can get wins to show value to others. Spellmeier recommends finding something measurable, even if small, instead of relying on anecdotal evidence.
- Avoid overlooking the simple things. Sometimes staff or clinicians simply do not know which tab or URL to go to. Document these details and communicate them early on.
- Look for opportunities to automate and simplify. Sometimes, an organization’s login process requires a person to manually set up each user account. Can these types of steps be automated or semi-automated?
- Create awareness in your team of the ripple effects an existing workflow has. In one case, Spellmeier needed to teach nurses to pull their own records because their usual process was to call an on-call physician and ask the physician to look up the patient’s information through the HIE and send it to them. In another example, Spellmeier helped an organization list their top ten facilities requesting records from the HIM department and engaged the requesting facilities to use the HIE to reduce HIM workload.
- Arrange training so that it is as easy as possible and does not cause undesirable side effects, such as overtime or other inconveniences. This arrangement could include producing and providing on-demand training videos or offering sessions during all necessary shifts to make attendance easier. You could also produce printable job aids or quick tip sheets specific to departments. Some people do better when they have something in their hands at the time they are planning to use a given workflow.
- Show organizations that their end-users are logging in and using the HIE’s tools. Periodic reporting or dashboards showing usage trends can help spur adoption and engagement.
- Ensure that training is followed by incorporating HIE usage in daily workflows and make that usage a habit for as many individuals as possible. It is generally not sufficient to conduct a demonstration and train people to use a given tool or solution. In one example, Spellmeier compared “before and after” reports showing active users and sessions before workflow integration and after. Spellmeier reported a 60% increase in monthly sessions after she was engaged.

Spellmeier suggested that organizations should align their strategies with regulatory requirements and plans. Staying up to date and advising member organizations of the likely impact of proposed legislation is an important part of an HIE’s activities. KHIN works to keep its members informed of such policy and regulatory changes. It distills potential impacts into easy to understand summaries and works with member organizations to create plans that respond to proposed changes, helping them make smooth adjustments over time.
As policies and public health priorities change over time, the workflow specialist’s role should include participation in such discussions and planning sessions. It could very well be the case that regulatory changes lead to modifications in using HIE data and services, and that fits squarely into the realm of responsibility of the workflow specialist.
How New York Boosted Care Coordination for Its Homeless Population Through Patient Matching

- Date: Tuesday, September 15, 2020
- Presenters:
- Thomas Moore, Senior Vice President, Innovation, Healthix
- Sana Ali, MS, MPH, Product Manager, Innovation, Healthix
- Mark LaRow, CEO, Verato
- Overview: In the final session of SHIEC 2020, leaders from Healthix and Verato discussed a joint applied research project to improve the identification and early detection of potentially homeless or unstably housed individuals.
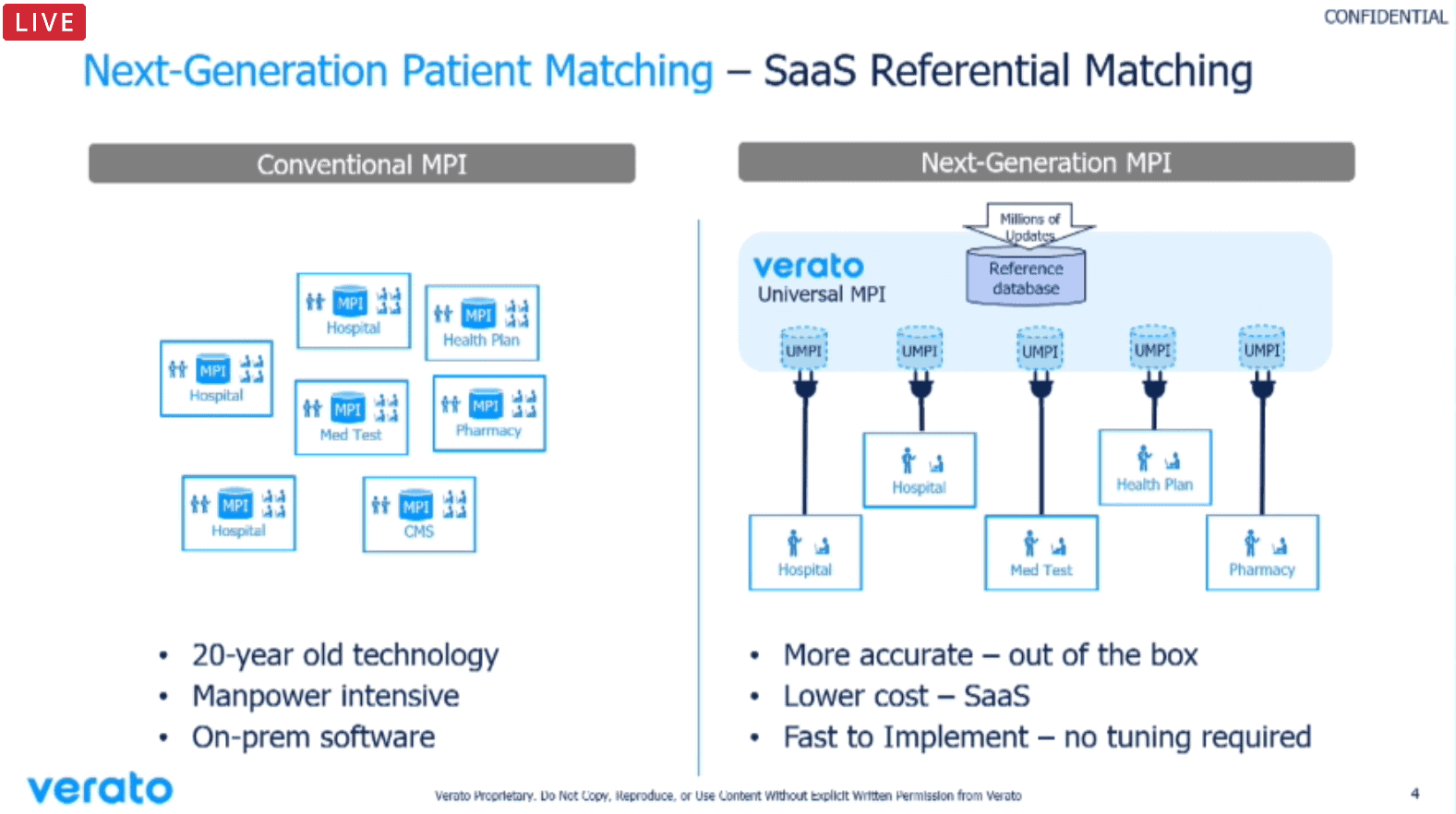
To start the presentation, Mark LaRow from Verato provided a brief history of patient matching. Historically, HIEs have used probabilistic matching based on demographic information provided in isolation and at the time of a given event or episode of care. Matching relied on evaluating the provided demographic information against locally known patient identities.
The next generation of matching technology adds a broader set of public and private identifying information to augment the standard probabilistic approach. The result is a more triangulated identification solution that takes advantage of information about a patient’s known identifiers and historical information (from sources such as Equifax, TransUnion, Experian, and LexisNexis) in addition to local/regional identification information.
LaRow explained that Verato’s matching is done in the cloud, resulting in savings for organizations relative to maintaining on-premise and local-only matching solutions. Another advantage of the Verato model is that as niche use cases are worked out with clients, the resulting improvements or new features are easily rolled out and made available to all clients.
In today’s example, Verato is supporting Healthix and learning with them as their project unfolds. They hope to make new and more accurate approaches to identifying homeless patients available to all of their clients.
Sana Ali from Healthix provided an overview of Healthix, which supports data and care initiatives for over 20 million people, and its homeless patient identification project.
Healthix is working on a variety of initiatives for clinical care, population health, public health, research, and direct to consumer engagement. In addition to services that HIEs commonly provide, Healthix has been working to share pertinent longitudinal patient record information to life insurance underwriters to assist in more accurately determining risks.
Ali further described the homeless situation in New York City. Homelessness in the city has reached the highest levels since the Great Depression. The number of homeless New Yorkers, a large number of whom are living with some form of mental illness, are sleeping in shelters every night at a rate 59% higher than ten years ago.
Compared to homeless families, homeless single adults have much higher rates of serious mental illness, addiction disorders, and other severe health problems. Since many of these individuals lack a safe place to store medications properly, high blood pressure, diabetes, and asthma tend to be worse and more difficult to manage.
The goal of the Healthix project was to improve the health outcomes of homeless and unstably housed persons by developing services and products for better care management/coordination. Specifically, the project sought to identify accurate proxies for homelessness, improve the linking of homeless patient records, and support effective and coordinated interventions and care management.
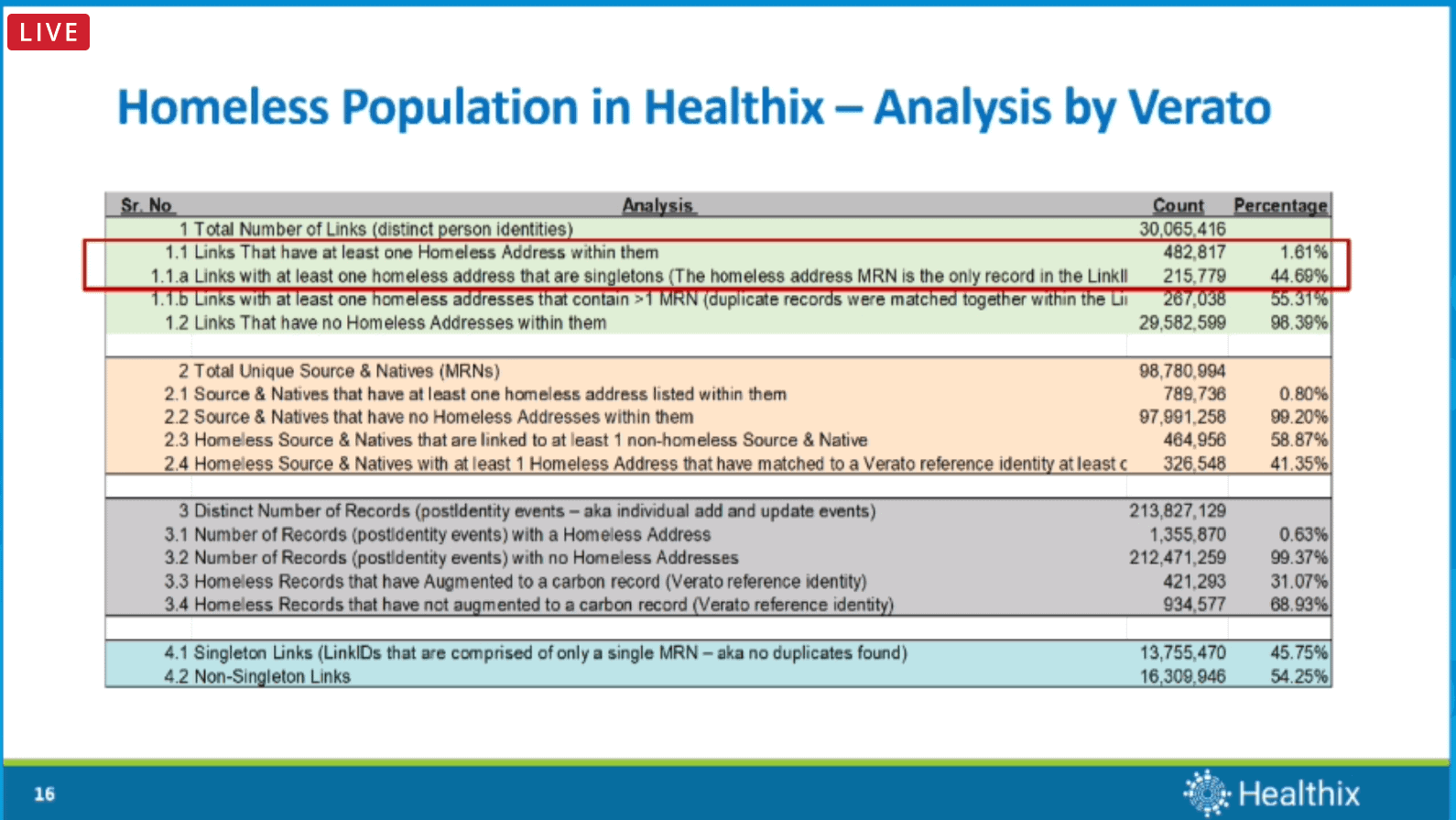
Even with advanced technology such as Verato’s, homeless patients are still difficult to match and track over time, chiefly due to lack of a primary address. Since homeless patients sometimes provide a proxy address such as a government building or a homeless shelter, Healthix sought to identify and flag them when given a patient’s primary address. Healthix also evaluated the number of times a specific address was given by more than one person to determine whether to include that address as a potential address used by homeless individuals.
The project received substantial support from participants and public health officials. Healthix formed an advisory group to assist in guiding the project and the use of the resultant data. The Healthix team reported learning many important pieces of information from the advisory group, such as how to distinguish between those who have been homeless for a shorter period of time, those who have been homeless on a regular basis, and the care protocols pertinent to these different groups. They also found that families seeking shelter were more likely to use primary care or preventive services compared to single individuals. The team also explored the relationship between homelessness and the criminal justice system and have since begun developing plans to work more closely with corrections facilities to support care for homeless individuals.
To carry out the project’s goal, the Healthix team tagged homeless patients in the HIE, ran all of its MPI records against the newly created Homeless Registry, and flagged all records where the primary residential address matched one of the addresses in the registry. These records were then separated by the facility into separate files and sent to the advisory council (those working directly with the homeless population) for validation. Each entity validated their clients’ housing status using a variety of methods, including manual chart review, data exports, and analyses from EHRs or registration software. Not all patients could be validated as homeless through this pilot due to being unreachable for follow-up or were recorded as deceased.
Healthix then worked on alerts to notify care team members who might be treating the same homeless patient in different settings and specifically worked to develop their alerting capability for difficult-to-locate homeless patients. Healthix’s research showed that their matching methodology to identify homeless patients worked well in identifying as many homeless patients as possible.
 The team has developed predictive models that evaluate housing history over time to help providers identify patients at higher risk of homelessness and enable care team members to reach out to those individuals to offer assistance to avoid situations that might lead to homelessness.
The team has developed predictive models that evaluate housing history over time to help providers identify patients at higher risk of homelessness and enable care team members to reach out to those individuals to offer assistance to avoid situations that might lead to homelessness.
The Healthix and Verato teams ultimately found that using referential matching alone was sufficient to develop a working and actionable homeless registry. The matching technology performed well enough on its own without the need for manual augmentation efforts that required sifting through data. Knowing this, the teams can now turn their attention to other important parts of their homeless population initiative. Their work can also be applied to surveillance opportunities and hypothesis testing.
HIEs are encouraged to continue to think about corner cases where advanced matching technologies can be improved or tuned to leverage automation and AI or predictive modeling to solve other real-world problems that HIE member organizations struggle to handle manually today.
| Week One Summary | Week Two Summary | Week Three Summary | Week Four Summary |
|---|

Thank you for joining during these five weeks of SHIEC 2020. Until next year!
J2 Interactive is an award-winning software development and IT consulting firm with a specialty in customized solutions for HIEs. Read about HIE platform migration.
We would be happy to have a no-obligation discussion about your HIE’s needs with you.



