Summaries by Nathan Elliott. Formatting and editing by Madeline Rizzo
| Day One Summary | Day Two Summary | Day Three Summary |
|---|

The Strategic Health Information Exchange Collaborative (SHIEC) is a national collaborative that represents health information exchanges (HIEs), associated organizations, and strategic business & technology partners.
2021 marks the seventh SHIEC conference. We are excited to be both back in person and viewing the sessions virtually. Join us over the upcoming days as we recap selected sessions from this year’s events!
2021 SHIEC Conference Welcome & Opening Remarks

- Date: Monday, August 16, 2021
- Presenters:
- Lisa Bari, Interim CEO, SHIEC
- Melissa Kotrys, CEO, Contexture | Board Chair, SHIEC Board of Directors
- Craig Brammer, CEO, The Health Collaborative
- Overview: Lisa Bari, Melissa Kotrys, and Craig Brammer open 2021 SHIEC with discussions on sponsorships, new organizations, upcoming presentations, the Keith Hepp Memorial Fund, and the future of health information exchange.
Lisa Bari, SHIEC’s Interim CEO, kicked off the 7th annual SHIEC conference with words of welcome, wayfinding, and anticipation about this year’s themes. Lisa thanked this year’s sponsors, including J2 Interactive—the day’s lunch sponsor.
 Bari spoke about this year’s hybrid conference model and how SHIEC is excited about the possibilities for continuing versions of it in the future. This year, SHIEC expects over 200 people to attend virtually.
Bari spoke about this year’s hybrid conference model and how SHIEC is excited about the possibilities for continuing versions of it in the future. This year, SHIEC expects over 200 people to attend virtually.
Melissa Kotrys thanked Lisa for her work this past year to continue SHIEC’s growth and advance its relevance during heightened interest in health information exchange in the wake of the global COVID-19 pandemic. Kotrys spoke about her own organization’s recent merger and launch as Contexture—a term that represents what is needed from all HIEs and networks today. By definition, contexture is the state of weaving or linking together components to create a connected whole or fabric. One of the major themes of this year’s conference is exploring models for industry affiliations, regional and national alignment on the things that matter most to all of us, and creative partnerships.
This year’s presentations will share insights and experiences that help articulate the need for local implementation of HIE, even when decisions are made to scale and share technology and national standards for data and data quality. One of the most valuable contributions of an HIE is having local or state-level trust and relationships to respond to needs and priorities that local officials and communities deem most valuable. It is difficult to respond to these needs with a single top-down solution across the country. Even though we, as an industry, are increasingly taking action to consolidate, partner, and expand to serve broader markets, we must be mindful not to focus on models that ignore the demand for highly customized programs and services at the state and local levels.
In keeping with the theme of affiliations and shared directions, Bari announced the merger of SHIEC and the Network for Regional Healthcare Improvement (NRHI) under the new name of Civitas, a Latin word meaning community and fellowship. More information can be found at the newly launched Civitas website. Future SHIEC activities and communications are expected to be provided under the Civitas brand.
To speak on behalf of NRHI, Craig Brammer shared a story about researchers in the mid-1900s. They observed native tribes and their social behaviors when functioning as individual tribes and when faced with a larger challenge that no single tribe could solve on their own. The researchers found that tribes that otherwise would spar and compete came together as a cohesive whole to respond to their shared challenge, despite their day-to-day differences and different priorities.
Brammer felt that this illustrated the current state of health information exchange today. Spurred by the COVID-19 pandemic but already underway for many in the industry, organizations are now taking action to work together on common problems that affect us nationally while maintaining local loyalty and different day-to-day priorities.
 Brammer also announced the Keith Hepp Memorial Fund to help bring young health IT professionals to industry events. Keith had a lifelong commitment to helping youth find career opportunities in health IT, and this fund continues that tradition. Brammer encouraged the audience to think about individuals who would benefit from this important new leadership development fund.
Brammer also announced the Keith Hepp Memorial Fund to help bring young health IT professionals to industry events. Keith had a lifelong commitment to helping youth find career opportunities in health IT, and this fund continues that tradition. Brammer encouraged the audience to think about individuals who would benefit from this important new leadership development fund.
At the end of the presentation, Bari retook the stage and thanked all of the individuals who helped bring SHIEC and NRHI together and launch Civitas as a combined voice of influence at the national level. Bari again noted the criticality of “swimming in the same direction on the things that matter most to us,” even as consolidation efforts are showing up in all corners of the industry today. Engagement and participation are essential to the success of Civitas members. Bari concluded with an invitation to find opportunities to get involved and provide feedback to inform the next wave of change for the HIE landscape.
SHIEC Conference Opening Keynote

- Date: Monday, August 16, 2021
- Presenters:
- Lisa Bari, Interim CEO, SHIEC
- Micky Tripathi, Ph.D. M.P.P., National Coordinator, Office of the National Coordinator for Health Information Technology (ONC), U.S. Department of Health & Human Services
- Overview: Micky Tripathi talks with Lisa Bari about ONC priorities, data/process gaps that must be solved to improve interoperability, and the relevance of USCDI and its upcoming extensions as a baseline for information sharing into the future.
Lisa Bari, the interim CEO of SHIEC, opened the session with an introduction for today’s speaker, Micky Tripathi, National Coordinator at the ONC. The session took the format of a Q&A conversation between Bari and Tripathi.
 Tripathi spoke about his background in health IT. Specifically, he spoke about his experience as a consultant with the Boston Consulting Group a few decades ago, at which time he was assigned to a project in Indianapolis to help form a business plan and launch a health information exchange. When that first project wrapped up, BCBS of Massachusetts announced a $50 million pilot project in the IT space that Micky saw as a great opportunity to return to his home state and leverage what he learned in Indianapolis. He has been involved in healthcare IT since then.
Tripathi spoke about his background in health IT. Specifically, he spoke about his experience as a consultant with the Boston Consulting Group a few decades ago, at which time he was assigned to a project in Indianapolis to help form a business plan and launch a health information exchange. When that first project wrapped up, BCBS of Massachusetts announced a $50 million pilot project in the IT space that Micky saw as a great opportunity to return to his home state and leverage what he learned in Indianapolis. He has been involved in healthcare IT since then.
Tripathi offered his take on the importance of dynamic growth and agility in today’s environment. He discussed the importance of expecting to continue to change and evolve. Market influences, policy, public health threats, and other factors all continue to change rapidly, which means HIEs and networks must be ready to keep adapting for the foreseeable future. A major part of that adaptation is continuing to experience and test new trust models and value-add services at the local level that fill gaps for stakeholders. Organizations can look to TEFCA as a “baseline” for interoperability, but the real value for stakeholders is the mix of services delivered by the HIE beyond simply moving commonly defined data to different destinations. It is the “last mile” services that will continue to make HIEs valuable—making affordable connections available where there have been none to date.
Tripathi mentioned that the ONC’s goal is to accelerate implementing solutions that span administrations. There is bipartisan support for healthcare priorities that range from enhancing and clarifying information blocking enforcement and disincentives to articulating how TEFCA can help fill gaps in the marketplace.
The ONC is being careful to define what it can directly control and what it might be able to influence appropriately. There are strict processes in place that must be followed at the federal level. Some of the areas of focus for the ONC include data and process gaps. In some cases, needed data is not curated well, leaving it incomplete or disjointed. In other cases, process gaps, such as lab staff not asking detailed Social Determinants of Health or other helpful questions as they take a specimen, contribute to missing insights. Process changes could lead to better care and more robust use of existing technologies.
 There is a major focus on the United States Core Data for Interoperability (USCDI) and leveraging this standard by adding to it over time. Tripathi’s office is pushing hard to include SDOH and Sexual Orientation, Gender Identity and Expression (SOGIE) data as part of USCDI.
There is a major focus on the United States Core Data for Interoperability (USCDI) and leveraging this standard by adding to it over time. Tripathi’s office is pushing hard to include SDOH and Sexual Orientation, Gender Identity and Expression (SOGIE) data as part of USCDI.
The ONC is also working with the CDC to make lab data more interoperable and with the CMS on quality-focused USCDI extensions. The intent of extending USCDI is to provide an “agnostic” baseline of data that should be widely available, regardless of individual use cases. It represents a floor, not a comprehensive list, but creating the right floor is important to accelerating useful information sharing. Moving data is necessary, but providers and public health officials are increasingly focused on data that is directly actionable and in eliminating the noise.
As HIEs talk about nurturing relationships at the local, state, and national levels, the ONC is taking similar steps internally between federal agencies. Much of Tripathi’s focus has been on working with other agency leaders to identify and articulate shared strategic priorities that lead to collaborative alignment on tackling challenges that might be larger than any single agency can solve.
Update from Sequoia / TEFCA

- Date: Monday, August 16, 2021
- Presenter: Mariann Yeager, CEO, The Sequoia Project
- Overview: Mariann Yeager speaks about the accelerated TEFCA timeline to implementation, QHIN Technical Framework standards and expectations, and how the public can engage in the process prior to the anticipated release of final documentation in Q1 2022.
Mariann Yeager, CEO of The Sequoia Project, spoke briefly about efforts to accelerate the timeline for implementing TEFCA and described both timeline and public feedback considerations. Specifically, there will be a webinar series to engage the public this summer and fall, with the goal of publishing final versions of documents in Q1 2022, followed by roll-out and onboarding.
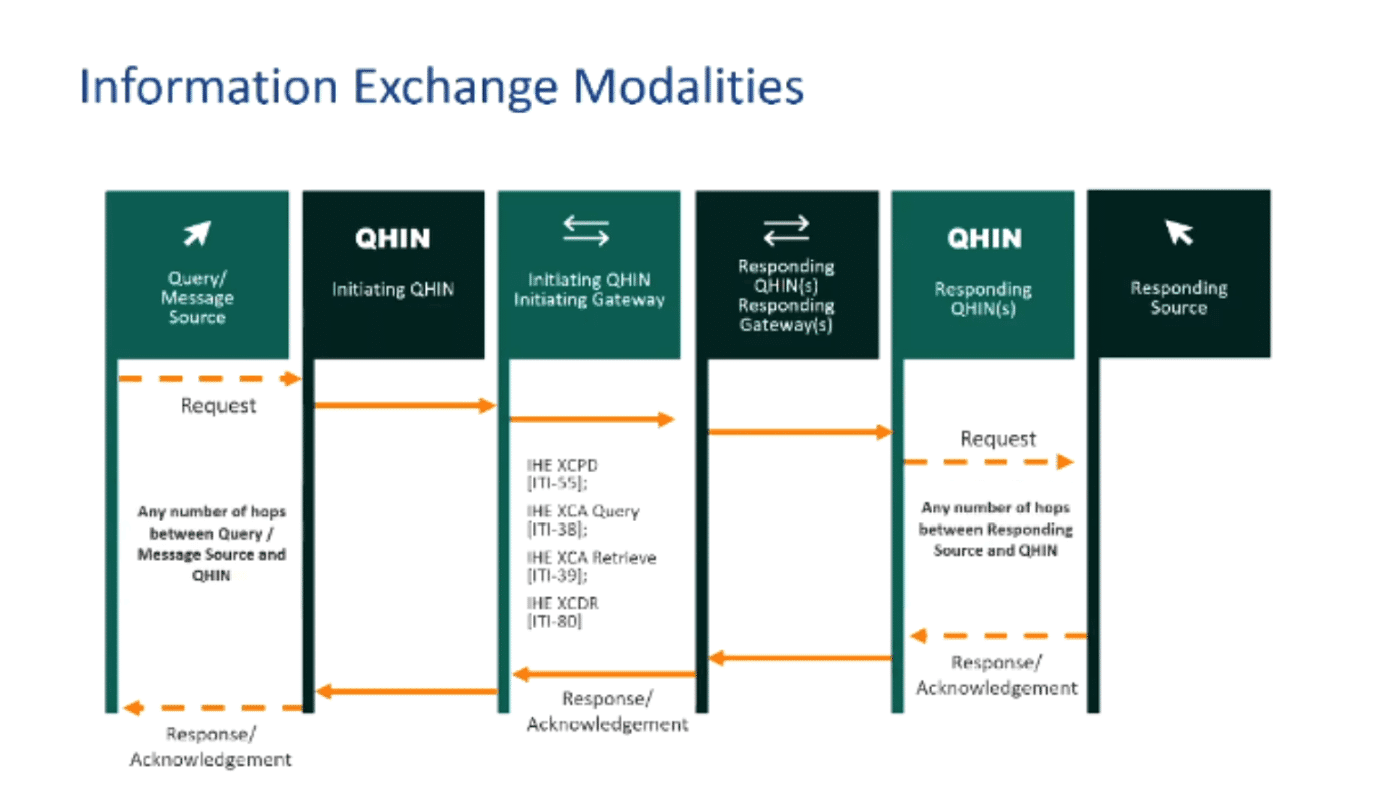 QHINs will feature prominently, and a significant amount of work has been done to help define how QHINs will operate, the standards QHINs will need to use, and the level of scrutiny and accountability to which QHINs will be subject. The bar is expected to be quite high.
QHINs will feature prominently, and a significant amount of work has been done to help define how QHINs will operate, the standards QHINs will need to use, and the level of scrutiny and accountability to which QHINs will be subject. The bar is expected to be quite high.
Additional work has been done to define message transaction protocols between QHINs. While QHINs might support a variety of connections and message transfer standards with their members, QHINs will rely on two major modalities: query-based exchange (IHE XCPD and IHE XCA) and push-based message delivery (IHE XCDR). More details will be provided during future informational webinars.
Yeager commented that most of the requirements would be at the QHIN level, with some number of flow-down provisions for participants, such as C-CDA standards, Access Consent Policy handling, USCDI data classes/elements, audit logging, core demographic data, and enforcing TLSv1.2 between participants and a QHIN.
The Sequoia Project will provide a roadmap for FHIR as part of the published version of the QHIN Technical Framework (QTF). One of the key challenges of incorporating FHIR is the multi-hop nature of QHIN architecture.
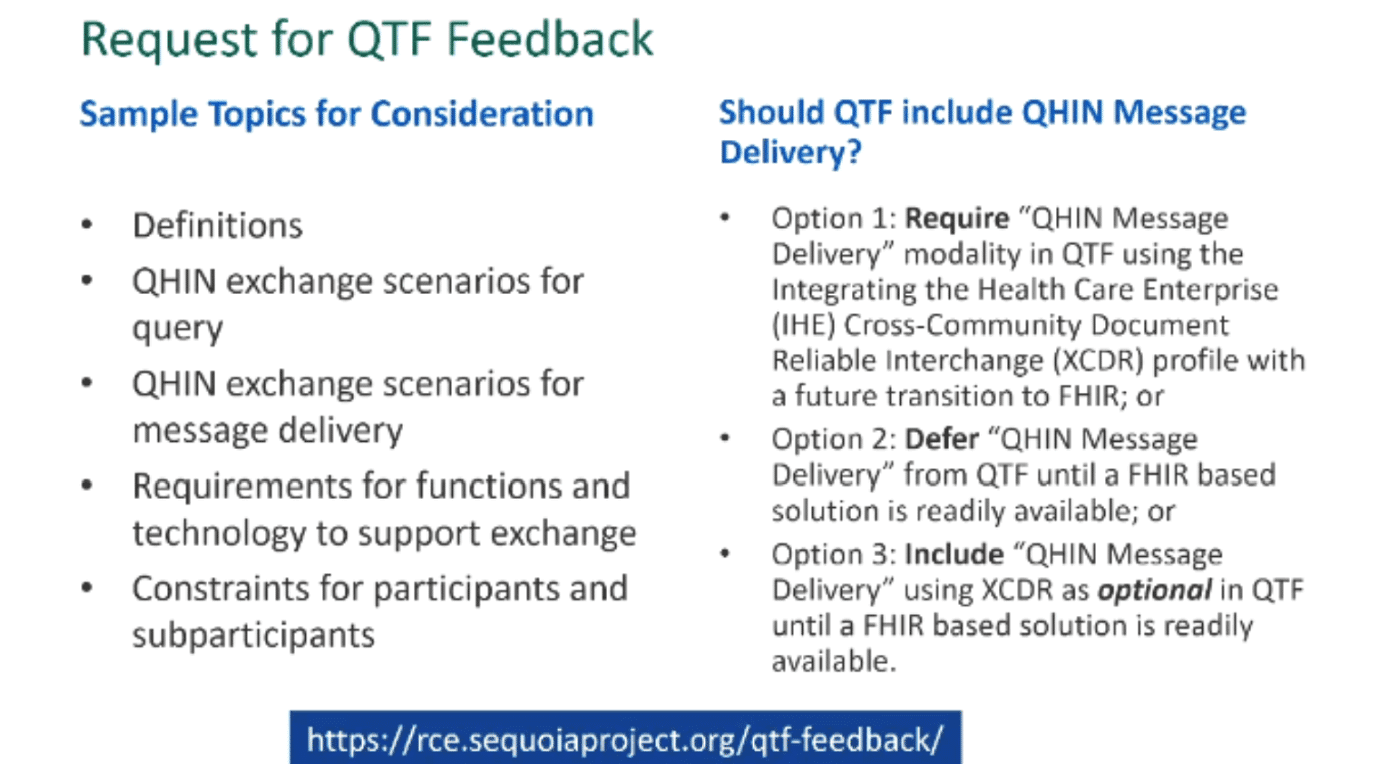 Feedback is requested on the QTF, which can be submitted here.
Feedback is requested on the QTF, which can be submitted here.
Yeager reminded the audience that those considering QHIN status must be prepared for a higher level of investment to meet the security, privacy, performance, and other expectations of QHINs relative to participants. Organizations will need to carefully consider their ability to sustainably meet these heightened requirements.
Multi-State Affiliations

- Date: Monday, August 16, 2021
- Presenters:
- David Horrocks, President & CEO, CRISP
- Don Rucker, MD, former National Coordinator, Office of the National Coordinator for Health IT (ONC)
- Lisa Bari, Interim CEO, SHIEC
- Morgan Honea, Executive Vice President, Contexture
- Overview: David Horrocks, Don Rucker, Lisa Bari, and Morgan Honea discuss the emerging trends pertaining to consolidation and affiliations in the HIE industry.
Dr. Rucker opened the presentation by speaking about the balance between federal policy (which can lead to mismatched priorities at the local or state level) and the need for a highly diverse body of information exchange contributors. These information exchange contributors include nursing homes, agencies, and non-profits involved with SDOH, as well as patient-generated or patient-contributed information.
 Dr. Rucker also argued the need to apply technologies to conduct more proactive disease surveillance with data. The fact that we still rely on 19th-century disease reporting methods tells us that we can and should do better.
Dr. Rucker also argued the need to apply technologies to conduct more proactive disease surveillance with data. The fact that we still rely on 19th-century disease reporting methods tells us that we can and should do better.
David Horrocks then talked about CRISP’s role as more of a public utility and shared his experiences branching out to Washington DC after connecting all of the hospitals in Maryland. What he found was that Maryland hospitals wanted to go in different directions than DC hospitals, which meant that while it was certainly possible to share platforms, talent, and support services, there still needed to be a local relationship between the HIE and a given jurisdiction, complete with separate boards and their own local connections.
Morgan Honea offered insights from his experience moving to a multi-state collaborative and expressed that the decision about defining geographies is often different as you move across the country.
The panelists elaborated on this point and said that, in some cases, health systems, city boundaries, commuting arrangements, natural boundaries, and other factors might determine whether service areas can or should be defined by state boundaries only. In some cases, large health systems might have a significant presence in multiple nearby states, making it more logical to define a multi-state service area for an HIE or closely affiliated HIEs. In other instances, there could be enough geographic, transportation, or other forms of separation to decide that state boundaries make the most sense for a given population.
 The group discussed the fact that defining these boundaries is still in flux today, especially because of the need for national alignment on standards, data quality, and interstate patient record sharing. The need to partner closely with government organizations and align with concepts such as QHINs are causing some to work toward broader affiliations. As HIEs work through determining the “right” size and scope for their organization, the general feeling is that in many cases, the appropriate size is somewhere between state and national, i.e., a mix of state-level HIEs and multi-state regional HIEs or networks where patient activity or other patterns indicate greater efficiencies across state lines. Some on the panel felt that it is difficult to provide efficiencies at levels smaller than the state level.
The group discussed the fact that defining these boundaries is still in flux today, especially because of the need for national alignment on standards, data quality, and interstate patient record sharing. The need to partner closely with government organizations and align with concepts such as QHINs are causing some to work toward broader affiliations. As HIEs work through determining the “right” size and scope for their organization, the general feeling is that in many cases, the appropriate size is somewhere between state and national, i.e., a mix of state-level HIEs and multi-state regional HIEs or networks where patient activity or other patterns indicate greater efficiencies across state lines. Some on the panel felt that it is difficult to provide efficiencies at levels smaller than the state level.
Even in collaborative arrangements, however, there is still local variation. Honea talked about differences in priorities between Arizona and Colorado within the newly formed Contexture. Arizona, for example, has invested heavily in building its innovative behavioral health solutions. Colorado is now learning from what Arizona has done, but it is not a guarantee that Colorado will copy Health Current’s original model precisely. In other areas such as accounts payable, there was a clear opportunity to simplify and streamline. Between Health Current and CORHIO, Honea said that they needed to process over 1,000 invoices each billing cycle. Cost savings were in order, and consolidating functions like that made the most sense at a multi-state level.
The take-away seems to be Lisa Bari’s earlier statement in the day: swimming in the same direction on the things that matter most to us, but allowing flexibility to go different directions for specific services at the local level.
Dr. Rucker commented on the challenge of not having a clearly defined privacy model. Ultimately, privacy laws are at the state level, and multi-state affiliations will have to work through this. He also shared his opinion that federal rules lead to information blocking and that consumers are eager to make data more accessible, just like they have with banking and other aspects of their lives. The challenge, in Dr. Rucker’s view, is needing to rely on the federal government to fix the policies that still encourage information blocking and, by extension, reluctance to engage in meaningful partnership and multi-state affiliations.
North Dakota Health Information Network Partnering with Public Health: Lessons Learned in a Pandemic

- Date: Monday, August 16, 2021
- Presenters:
- Shila Blend, Health Information Technology Director, NDHIN
- Eric Hieb, Technology Lead, NDHIN
- Benjamin Schram, Surveillance and Electronic Reporting System Coordinator – Epidemiologist III, NDHIN
- Overview: NDHIN’s Shila Blend, Eric Hieb, and Benjamin Schram discussed their experience with leveraging ADT feeds to improve disease-based monitoring and alerts and how they were affected during the COVID-19 pandemic.
North Dakota HIN (NDHIN)’s Shila Blend, Eric Hieb, and Benjamin Schram presented their experience with leveraging ADT feeds to improve disease-based monitoring and alerts. For example, where autism diagnoses are available in ADTs (an area of opportunity for improvement), alerts can be sent to the state’s case management system to create or update cases automatically to enhance encounter awareness and support follow-up efforts.
 North Dakota also leverages ADTs for other diseases such as possible COVID-19 encounters. These alerts provide up-to-date insight into hospitalizations and patient deaths.
North Dakota also leverages ADTs for other diseases such as possible COVID-19 encounters. These alerts provide up-to-date insight into hospitalizations and patient deaths.
The lesson learned, however, is that having many alerts can become overwhelming. In North Dakota’s case, one staff member received and needed to review a new alert for every patient each day, even if their status had not changed. The state gradually moved toward monitoring discharges, specifically, to report accurate numbers across the state and thinned out their alert generation criteria.
North Dakota also leveraged NDHIN to find patient contact information during the pandemic response. This approach proved essential in outreach efforts. In some cases, this was a phone number or new address. In other cases, emergency contact information was available to help locate patients.
The state also worked with NDHIN to leverage lab data from multiple sources, given the fact that not all testing sites had the IT infrastructure necessary to capture important tracking or results data at the time of testing. This capability was of great value to the state. Eric Hieb from NHDIN stressed the importance of maintaining strong working relationships between HIEs and the state to prepare data for useful scenarios and to be the first place states go to ask for help with data is needed.
Congressional Staff Panel Discussion: Health IT and Data Modernization Policy Today and Tomorrow


- Date: Monday, August 16, 2021
- Moderator: Lindsay Austin, Principal, Troutman Pepper Strategies
- Presenters:
- Colin Goldfinch, Deputy Health Policy Director at the Senate Committee on Health, Education, Labor, and Pensions for Chairwoman Patty Murray (D-WA)
- Aliza Silver, Senior Health and Oversight Counsel at the Senate Committee on Health, Education, Labor and Pensions for Ranking Member
- Richard Burr (R-NC) Orriel Richardson, Health Counsel at the House Ways and Means Committee, subcommittee on Health, for Chairman Richard Neal (D – MA01)
- Stuart Portman, Senior Health Policy Advisor at the Senate Committee on Finance for Ranking Member Mike Crapo (R-ID)
- Overview: Congressional staff members provide updates on the current priorities of the officials with whom they work. The panelists offer key insights into some of the collaborations underway at the federal level that could affect the HIE community in the coming months.
Colin Goldfinch (Chairwoman Patty Murray, D-WA) began the session by noting the important investments in public health infrastructure that have been made in the past year. It is well known that state and local health departments operate on limited funding, but, to their credit, have been able to allocate resources to significantly enhance the readiness of public health systems in collaboration with HIEs to better respond to emergency situations.
Goldfinch also described priority topics including promoting health equity, improving maternal health outcomes, making clinical trials more representative, and supporting investments in public health infrastructure that help address specific inequities. Efforts are also underway to support the healthcare workforce and continue to reduce costs.
 Aliza Silver (Ranking Member Richard Burr, R-NC) discussed the improvements that are also ongoing at the federal level, especially where efforts are being made to intentionally avoid creating data silos at all levels. Unfortunately, different agencies can ultimately craft separate data sets that contribute to fragmentation in efforts to comply with requirements that might not be properly aligned from a policy perspective.
Aliza Silver (Ranking Member Richard Burr, R-NC) discussed the improvements that are also ongoing at the federal level, especially where efforts are being made to intentionally avoid creating data silos at all levels. Unfortunately, different agencies can ultimately craft separate data sets that contribute to fragmentation in efforts to comply with requirements that might not be properly aligned from a policy perspective.
Sen. Burr is currently focused on continuing to enable authorizations that were initially put in place as part of the 2005 Pandemic and All-Hazards Preparedness Act. These authorizations include supply chain and ensuring ready access to PPE and supplies that take advantage of federal purchasing power. Today, only about 4% of PPE is purchased through federal contracts.
There is also strong interest in the VALID Act and diagnostics reform.
From Orriel Richardson’s (Chairman Richard Neal, D-MA01) vantage point, there is a major focus on health inequities and using technology to pinpoint where those inequities occur. This technology can include impacts of such things as HIPAA waivers and understanding benefits and limitations. There is also interest in ensuring real-time data that is complete and accurate to facilitate government decision-making.
Governments are on the hook for making many decisions during times of crisis or rising threats and will increasingly require excellent data to quickly make sound decisions and avoid wasted time, wasted resources, and introducing possible harm. While the federal government has a major role to play in facilitating and reimbursing for new technologies, including telehealth services, it will not be up to Congress to directly dictate which services to offer through telehealth and related technologies.
According to Stuart Portman (Ranking Member Mike Crapo, R-ID), from a financing perspective, there is significant interest in identifying programs that were successful during the pandemic and on immunization initiatives. Congress is also learning from the pandemic where limitations have resulted in confusion or burden, such as the need for better reimbursement for e-consults for providers as part of a more comprehensive virtual care system.
Portman also discussed the looming challenges and constant presence in financing discussions of Medicare insolvency. When data comes in that suggests earlier insolvency, all discussions tend to go there, and progress is threatened on other high-priority topics.
The speakers generally agreed that data quality is a must moving forward. Data clean-up is a priority; it will not work for clinicians and care team members to have to sort through dozens of versions of similar data from multiple sources or be left having to try to reconcile incomplete data.
The industry should see quality data as necessary to smooth the transitions to quality-based payment programs of the future. Change will not necessarily be easy but will especially be problematic without clear and reliable data-driven insights to identify change opportunities and results of early transitions to new models.
The panel affirmed the notion that everyone now understands the value of health information exchange, and it is important to factor in its role in healthcare delivery and public health in the future.
Thank you for joining us for day one at SHIEC!
| Day One Summary | Day Two Summary | Day Three Summary |
|---|
J2 Interactive is an award-winning software development and IT consulting firm specializing in customized solutions for hospitals, labs, research institutions, and health information exchanges.
Our approach to design and development is rooted in a fundamental belief that systems succeed or fail based on how well they serve the people who depend upon them. Drop us a line to learn more.

