Summaries by Nathan Elliott. Formatting and editing by Madeline Rizzo
| Day One Summary | Day Two Summary | Day Three Summary |
|---|

The Strategic Health Information Exchange Collaborative (SHIEC) is a national collaborative that represents health information exchanges (HIEs), associated organizations, and strategic business & technology partners.
2021 marks the seventh year of SHIEC! We are excited to be both back in person and viewing the sessions virtually. Join us over the upcoming days as we recap selected sessions from this year’s events!
States, HIEs, and immunization information systems: The ONC IDEAS Program with ASTHO, SHIEC, AIRA, and AIM


- Date: Tuesday, August 17, 2021
- Presenters:
- Kate Ricker-Kiefert, State Health IT Policy Advisor, SHIEC
- Ryan Argentieri, Deputy Director, Office of the National Coordinator for Health Information Technology (ONC)
- J.T. Lane, Chief Population Health & Innovation Officer, Association of State and Territorial Health Officials (ASTHO)
- Rebecca Coyle, Executive Director, American Immunization Registry Association (AIRA)
- Claire Hannan, Executive Director, Association of Immunization Managers (AIM)
- Overview: Conference-goers hear from the ONC, AIRA, AIM, and ASTHO about the role of immunization programs at the federal and state levels, some of the challenges immunization registries face today, and the types of approaches HIEs can take to better align with both program leadership and the information they manage.
In February this year, the ONC launched the Immunization Data Exchange, Advancements and Sharing (IDEAS) program. Ryan Argentieri, Deputy Director of the Office of Technology for the ONC, explained the role of the program in identifying bright spots across the country in response to the pandemic. Specifically, her offices have been looking into where HIEs have had success with race, ethnicity, and situational awareness data, as a few current examples. Argentieri expects ongoing work in this area to bring more attention to the progress being made in areas that have perhaps been less visible and not well funded. The ONC advocates for building consensus and employing standards-driven approaches to address gaps by leveraging what is demonstrated to work well at a practical level.
The Association of Immunization Managers (AIM), headed by Claire Hannan, is a professional organization representing the 64 immunization programs across all 50 states, eight territories, and six major cities in the US. Hannan explained that AIM is an association much like SHIEC and provides support, coordination, and advocacy on behalf of its members.
Hannan discussed the level funding constraints of the immunization programs, all of which receive funding from the CDC’s National Center for Immunization and Respiratory Diseases (NCIRD). In most years, expenses rise for immunization programs as they do for the rest of the economy, but funding remains the same. Fortunately, immunization programs have seen some add-on funding specific to COVID-19 and the flu in the past year, given the significantly increased level of work to track results.
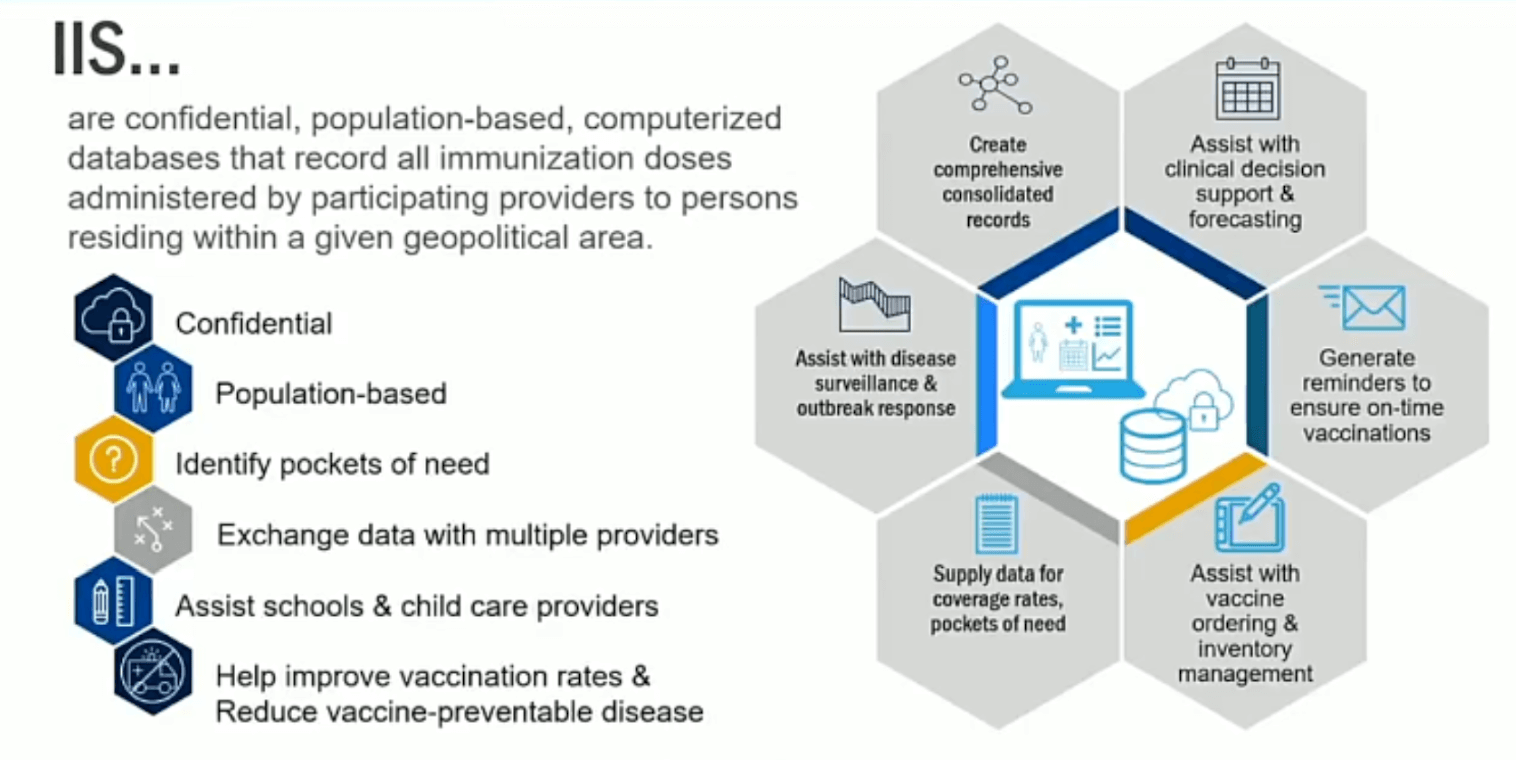
Immunization Program Managers are typically responsible for administering the Vaccines for Children Program, conducting outbreak control, developing strategies to increase coverage and reach in underserved populations, delivering immunization education and awareness building, and managing annual work plans and budget proposals. As COVID-19 emerged, additional duties included pursuing partnerships with new stakeholders beyond normal spheres of influence, expanding grassroots efforts at the local level to reach underserved populations, leveraging IT in more sophisticated ways to track vaccines and vaccinations, and upgrading state Immunization Information Systems (IIS).
 Hannan noted that the increased investment of time, money, and talent into the COVID-19 vaccine/vaccination data tracking and producing visualizations for both directly contributed to increased levels of success for COVD-19 vaccination efforts.
Hannan noted that the increased investment of time, money, and talent into the COVID-19 vaccine/vaccination data tracking and producing visualizations for both directly contributed to increased levels of success for COVD-19 vaccination efforts.
Rebecca Coyle from the American Immunization Registry Association (AIRA) provided an overview of her organization’s role in supporting the IIS component of state immunization programs. One notable challenge of coordinating data across states is that each state can house their IIS in different departments. Some have more direct control over changes or updates, while others require significantly more coordination between departments or offices when any IIS decisions need to be made, such as responding to the pandemic.
COVID-19 dashboards, for example, are fed by state IIS data. IIS also supports school vaccination programs and works with providers to enable query access to patient immunizations to facilitate care and planning. The association is working on improving standards and consistency across ISS instances. Some of the variations between states include:
- Some states have specific registries that others do not (e.g., newborn screening and lead screening).
- Local laws or policies might govern who can and cannot access data within or outside the state.
- Consent models tend to differ between states. While most are opt-out, some are still opt-in.
- COVID-19 reporting is mandatory, but other vaccines are not.
- Levels of system maturity and data quality might differ between ISS instances in different states.
Coyle felt that ironing out these inconsistencies will be critical to maturing these systems for more reliable and rapid use in the future. Funding tends to be “boom and bust” for immunization programs, with additional infusions of funding after public health emergencies are underway. Ideally, funding could be structured in ways that help prepare for modernization and maturity efforts before urgent demands arise.
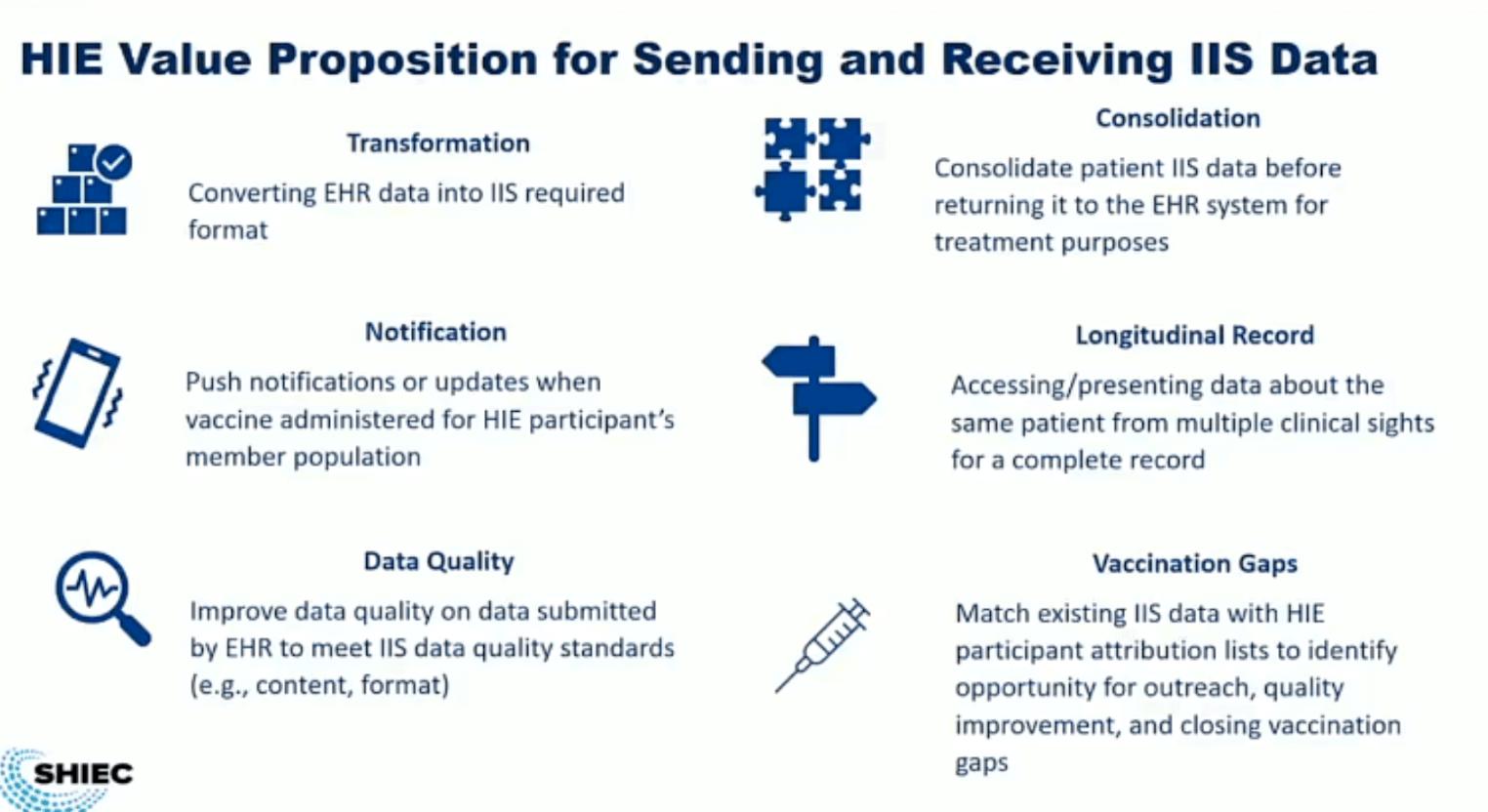 SHIEC’s Kate Ricker-Kiefert presented her take on some of the challenges that HIEs will need to consider in working with registries such as those for immunizations. HIEs come in multiple forms and governance and consent, for example, are not likely to line up with state-run registries in many cases. These variations will require intentional collaboration to resolve disconnects, especially for HIEs operating across state lines.
SHIEC’s Kate Ricker-Kiefert presented her take on some of the challenges that HIEs will need to consider in working with registries such as those for immunizations. HIEs come in multiple forms and governance and consent, for example, are not likely to line up with state-run registries in many cases. These variations will require intentional collaboration to resolve disconnects, especially for HIEs operating across state lines.
Some opportunities for HIEs to consider:
- Convert EHR data into IIS required format (some HIEs are doing this today).
- Improve the quality of data submitted by EHRs to meet IIS standards.
- Implement push notifications or updates when a vaccine is administered for an HIE participant’s member population.
- Consolidate patient data from ISS instance(s) before returning it to EHRs for treatment purposes.
- Match existing IIS data with HIE participant attribution lists to identify opportunities for outreach, quality improvement, and closing vaccination gaps.
J.T. Lane from the Association of State and Territorial Health Officials (ASTHO) mentioned that many of the barriers we face are less technical in nature and more political—this is why we continue to see challenging variations that hinder interoperability. He offered examples in California and Louisiana. In the former, permission to pursue initiatives needed to be secured up front. In Louisiana, projects can be initiated until or unless local or state governments disallow them. He has been encouraged to see more conversations and partnerships emerging, but more action-oriented discussions to make policy more flexible or aligned are still needed.
In keeping with the theme of the conference so far, relationship-building is key to the next phase of evolution for HIEs and the widening ambit of organizations with which HIEs will need to coordinate. One major challenge is that in some states, turnover in key positions is very high. Lane referred to a recent article citing one county-level health official retirement or resignation in Washington state per year, on average. In the past year, there have been nine. It is difficult to make progress when conversations and partnership negotiations have to start again with new players, which serves as a reminder to build deeper relationships in organizations (and across more organizations) rather than focusing on just one organizational contact at a time.
The Public Health Data Utility Model for HIE: A Post-Pandemic Statewide Vision


- Date: Tuesday, August 17, 2021
- Presenters:
- Jaime Bland, CEO, CyncHealth
- David Horrocks, President & CEO, CRISP
- Melissa Kotrys, CEO, Health Current
- Claudia Williams, CEO, Manifest MedEx
- Angie Bass, EVP, Velatura HIE Corp.
- John Kansky, President & CEO, Indiana Health Information Exchange
- Lisa Bari, Interim CEO, SHIEC
- Jess Kahn, Partner, McKinsey & Company
- Overview: Lisa Bari leads a panel of HIE leaders in discussing the current shift in identifying HIEs as health data “utilities.” The panelists provide their insights into what makes a health data utility and the work needed to shift from a more competitive and open market to one where HIEs are the go-to essential health data resource for providers, states, and a growing list of future stakeholders. In the words of Lisa Bari: “health data is infrastructure.”
In this session, panelists discussed the features of HIEs moving toward a “health data utility” model to help both private and public stakeholders better understand the value and position of HIEs in the healthcare space. Part of this effort is defining a particular identity that helps the public better understand how to engage with an HIE and differentiate HIEs from other solutions, such as EHR-based networks and state-run data repositories.
 Lisa Bari provided some initial thoughts, including the fact that the HIE community has stepped up in the last year to begin demonstrating value in ways that we did not see coming just a few years prior, including such things as vaccine credentialing. These actions speak to HIEs’ adaptability and that this is a critical time to take advantage of those successes and anchor HIEs in the minds of decision-makers across the country. What matters here is that HIEs are not just continuing to talk about doing more than moving data around—they’re starting to do a lot more in real life. One panelist felt that if HIEs do not use this time to extend their value and accelerate partnerships with critical stakeholders, the industry could be set back by as much as ten years and would have to re-start conversations with many important stakeholders.
Lisa Bari provided some initial thoughts, including the fact that the HIE community has stepped up in the last year to begin demonstrating value in ways that we did not see coming just a few years prior, including such things as vaccine credentialing. These actions speak to HIEs’ adaptability and that this is a critical time to take advantage of those successes and anchor HIEs in the minds of decision-makers across the country. What matters here is that HIEs are not just continuing to talk about doing more than moving data around—they’re starting to do a lot more in real life. One panelist felt that if HIEs do not use this time to extend their value and accelerate partnerships with critical stakeholders, the industry could be set back by as much as ten years and would have to re-start conversations with many important stakeholders.
Various features of HIEs, such as a health data utility, were discussed, including HIEs’ obligation to be mission-driven, serve the “last mile,” and provide services in places that are not “profitable,” or at least not entered into because of profit-seeking intentions. HIEs should ideally see themselves as more of a public good. Funding and sustainability are obviously important to an HIE, but HIEs should look to creative funding models and partnerships (such as with state Medicaid programs) that do not require the HIE to ignore or intentionally exclude segments of the population that they serve. Providers in any area should be able to turn on a machine and see useful patient data, not unlike turning on a light switch and expecting (and having) the light come on.
One essential element in moving toward a utility model is making sure that local communities embrace that image of an HIE. This goal will require some work, as HIEs need to be ready to explain both the similarities and important differences that make the “utility” argument understandable and acceptable. As HIEs enhance their presence as the service provider of choice for key programs or solutions (e.g., alerts or perhaps COVID-19 dashboards), HIEs need to encourage a wider variety of stakeholders in their communities to come to them to bolt on new solutions. This centralized staying power is what makes HIEs more of a utility. Originally, electricity, for example, could be acquired to power a light bulb. Think of the electricity that hospitals, households, companies, and public infrastructure today rely on for such a wide variety of needs and pursuits. Panelists believe this is the direction in which HIEs are moving.
The primary question, it seems, is exactly how to shift from what feels like a competitive, almost for-profit environment to one in which both private and public stakeholders assume that the HIE needs to survive financially and make provisions to ensure that future. At the moment, HIEs are still in a “sink or swim” mode; attempts are fully underway to help reshape that model to one of being essential to daily life for a wide variety of people. When HIEs achieve “essential,” it appears that they can then begin to call themselves more of a public utility.
Success and fruitful pilots seem to come from strong funding sources, such as payers and governments focused on paying for data specifically. California’s governor is considering mandates for payers and providers to contribute data for information exchange purposes. Such mandates appear to have a lot of support from the HIE community. These types of not-so-subtle nudges have helped HIEs accelerate participant and data growth in a number of states. The panel is looking for this continued growth to expand, and that sentiment has been echoed in other sessions during this year’s conference. The pandemic both pushed this goal forward in real terms for real projects and put the need for payer and public mandates far more into the spotlight for many.
Funding is always a challenge, so HIEs will need to work with their stakeholders to define the programs that are “essential” enough to be worth paying for now and into the future. Panelists felt that combining data from multiple sources is one way to move closer to being essential, but HIEs still need to spend more time carefully listening to what those paying stakeholders need to solve and what their gaps are. Combining data in isolation or for the sake of flexing an HIE’s ability to do so in a “build it, and they will come” manner appears to be far less promising. Carefully listening, curating, and intelligently leveraging data to solve real problems quickly and as precisely as possible reveals a more agreeable path to essentiality.
It also appears that the tone of engagement is an important factor as HIEs navigate these possibilities. Most stakeholders are more interested in being heard than in being sold something. Manifest Medex’s Claudia Williams commented that there is simply too much competitive jockeying in the market today and that HIEs must take responsibility for putting mission first and keeping those broader public obligations at the forefront in all conversations.
Another theme of the discussion (and the conference this year) is that federal, state, and local policies need to encourage and set the stage for rapid response and agility across state borders. Current variations tend to slow down progress and add significant layers of complexity to arriving at multi-jurisdiction solutions. Standardization, flexibility, and incentives to deploy solutions quickly at and below the federal level will help speed value demonstrations on the path to that hoped-for essentiality.
As Lisa Bari summed up, what we all need to understand and work into our conversations is that “health data is infrastructure.”
Public Health Needs Data, Healthy Data
- Date: Tuesday, August 17, 2021
- Presenters:
- Russell B. Leftwich, MD, FAMIA, Senior Clinical Advisor, Interoperability, InterSystems
- Nick Bonvino, CEO, Greater Houston Healthconnect
- Todd Rogow, President and CEO, Healthix
- Neil Sarkar, President and CEO, RIQI
- Overview: Panelists discuss success stories from three HIEs using InterSystems technologies.
Greater Houston Healthconnect’s (GHH) CEO, Nick Bonvino, opened the session with a presentation about the work GHH has done in the past year in collaboration with the University of Texas Health on COVID-19 outcomes. The goals of the collaboration included:
- Patient Cohort Construction – Leveraging HIE infrastructure and data to create cohorts of ethnically diverse COVID-19 positive patients in Texas and Louisiana
- Long-Term Surveillance – Long-term monitoring of clinical outcomes including mortality, heart, lung, blood, and kidney disease
- Predictors of Disease – Analyzing demographic, social, pharmacologic, and other predictors of mortality and morbidity

Two specific research projects were included: homeostasis, clotting, and outcomes (e.g., DVT, stroke), and IL-6 inhibitors as treatment and outcomes (e.g., death and length of stay). This COVID-19 outcomes research project has been one of the largest, with over 1 million patients. Results were published last autumn in PLOS One, and the collaboration was covered by Healthcare Innovation in June.
According to Bonvino, GHH was able to facilitate this research because so many connections were already in place and data was available to begin using, even before there were COVID-19 codes. By building a broad foundation of data from all possible sources, GHH was able to make rapid value-add pivots to help answer specific partners’ key questions. Foundational to this broad base of data is mastering patient identity and committing to investing in curating high-quality data.
Bonvino noted that having only a subset of a patient’s encounters drastically reduces the value of the data because only half of the patient’s story is known at the time it is needed. GHH also supported COVID-19 efforts by monitoring ADT feeds (GHH receives about 18 ADTs per second, on average) and offering a clinical viewer as a one-stop-shop for case investigations. Without such tools, case investigations can require people physically getting into cars and driving or calling to request records.
Neil Sarker, President and CEO of the Rhode Island Quality Institute (RIQI), presented the work that RIQI has done to advance artificial intelligence in healthcare in the past year. In partnership with the state government, RIQI developed a process to extract a lab-like feed from CCDs for COVID-19 identification in near real-time. The solution pushed COVID-19 alert data into a contact tracing system, which is still functioning in Rhode Island today.
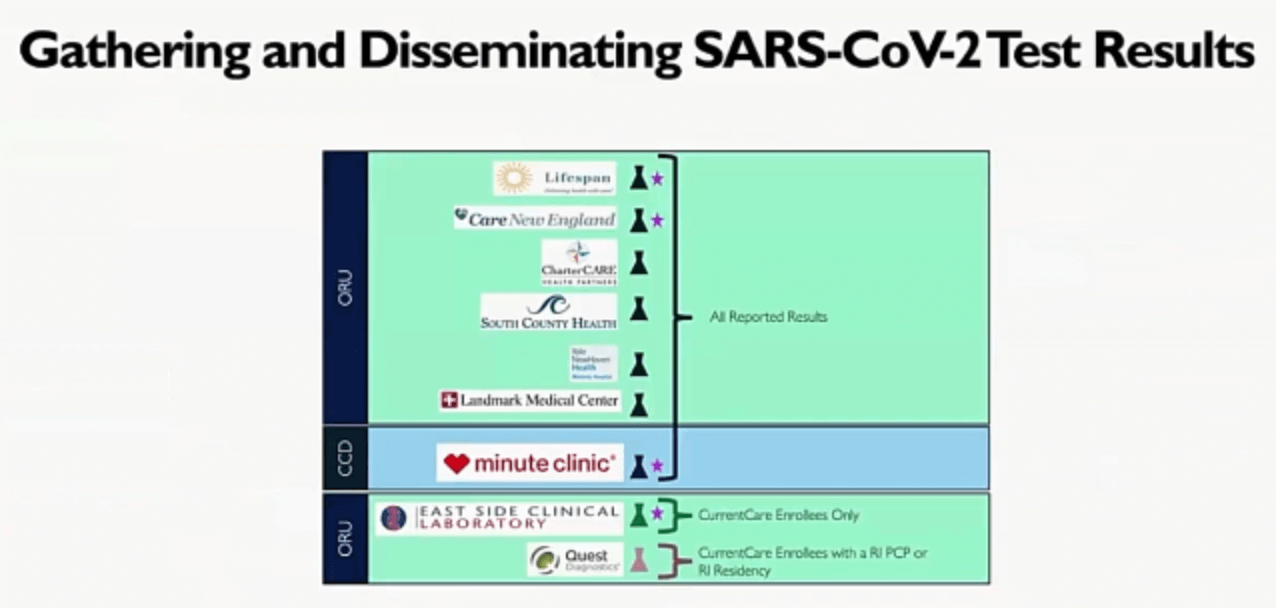 Providers also wanted to see COVID-19 test results, so RIQI built a solution that shows providers a combination of COVID-19 results (filtered by individual or result) and a Natural Language Processing-based method of flagging patients with encounters that potentially indicate COVID-19.
Providers also wanted to see COVID-19 test results, so RIQI built a solution that shows providers a combination of COVID-19 results (filtered by individual or result) and a Natural Language Processing-based method of flagging patients with encounters that potentially indicate COVID-19.
RIQI also found lower rates of testing and higher rates of COVID-19 among Latinx populations and is working with community resources to support improvements in testing and prevention outreach efforts.
Sarker noted that AI is not meant to be a replacement for providers. Physicians and care team members need to continue to do the things they are great at doing but leverage AI to help make the tedious and time-consuming tasks faster, more efficient, and ideally, more accurate.
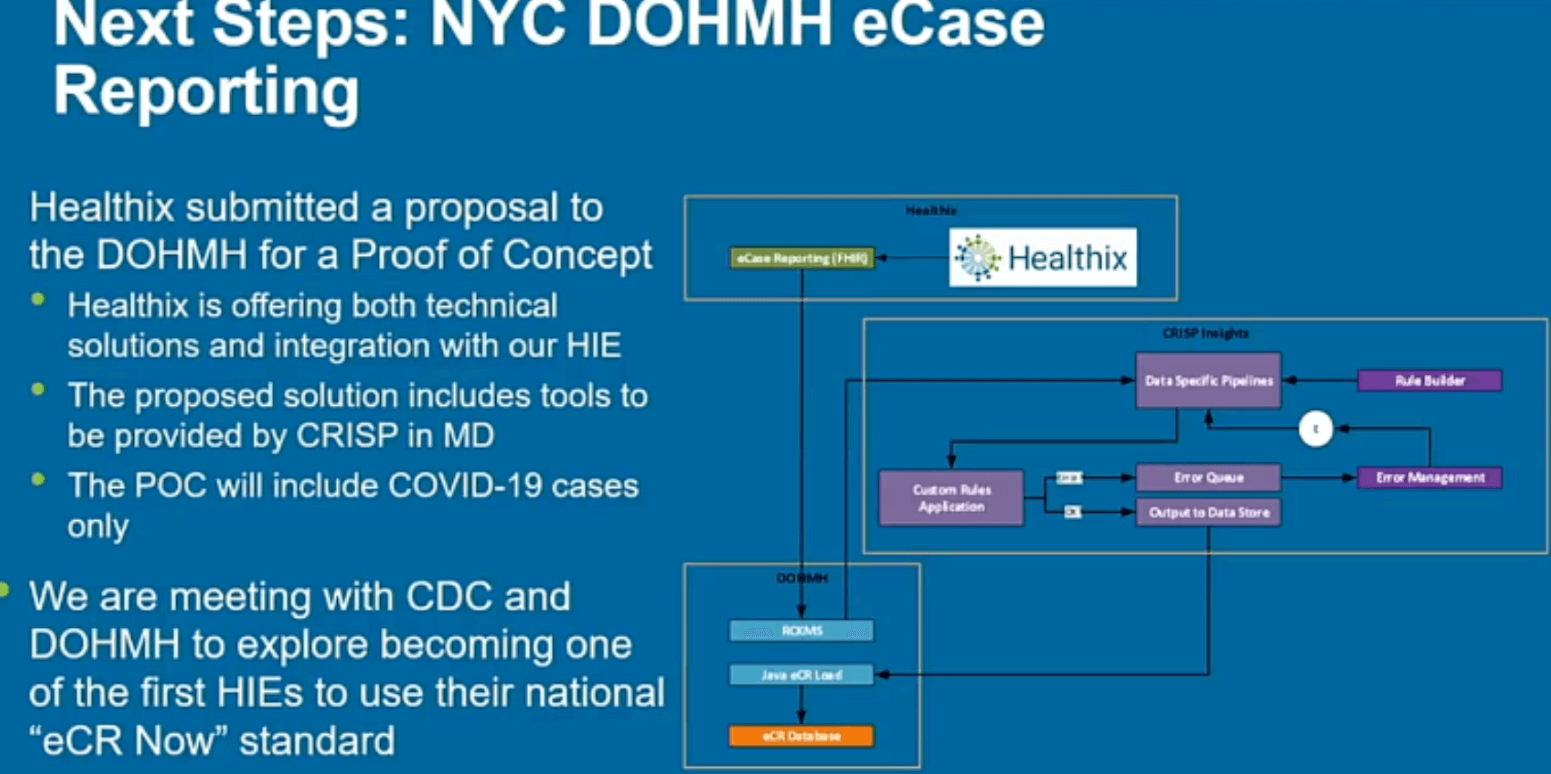
Todd Rogow, Healthix President and CEO, spoke about his organization’s work for COVID-19 mitigation and its collaboration with the New York City Department of Health and Mental Hygiene. Healthix supports over 18,000 clinicians and processes over 300 million messages per month. As a member of SHIN-NY, Healthix contributes to and benefits from statewide access to data. Healthix is also connected to other private HIEs and national networks.
 Healthix has supported a program for the Office of School Health seeking to provide outreach and care coordination for children between the ages of 6-18 with diagnoses of asthma, diabetes, or severe mental illness. As part of this cohort identification service for the city, Healthix found over 13,000 children with asthma that the city was not aware of and thousands of children with other diagnoses that will help the city with their school health programs. This collaboration is expected to expand in the future.
Healthix has supported a program for the Office of School Health seeking to provide outreach and care coordination for children between the ages of 6-18 with diagnoses of asthma, diabetes, or severe mental illness. As part of this cohort identification service for the city, Healthix found over 13,000 children with asthma that the city was not aware of and thousands of children with other diagnoses that will help the city with their school health programs. This collaboration is expected to expand in the future.
In addition to these initiatives, Healthix has a bidirectional exchange with the Citywide Immunization Registry (CIR). The CIR currently holds roughly 4.8 million records and over 75 million immunization events. All 81 public sites have reported that in the last six months, and 74% of private sites have reported in the same time period. The registry captures about 75% of all immunizations given. Healthix is actively engaged in assisting the city in identifying high-risk populations and targeting specific zip codes for vaccination and prevention efforts.
In terms of what is next for Healthix, Rogow said his organization has submitted a proposal to the Department of Health and Mental Hygiene to leverage a tool provided by CRISP to improve monitoring for COVID-19 patients. Healthix is meeting with the CDC and the Department of Health and Mental Hygiene to explore becoming one of the first HIEs to use the national “eCR Now” standard.
SHIEC Achievement Awards

- Date: Tuesday, August 17, 2021
- Presenters:
- Lisa Bari, Interim CEO, SHIEC
- Melissa Kotrys, CEO, Contexture | Board Chair, SHIEC Board of Directors
- Overview: Every year, SHIEC recognizes members of the HIE community for their contributions across seven domains. We join SHIEC in applauding the work these fellow industry leaders continue to do to improve the lives of those touched by an HIE.
Innovation AwardCRISP |
 |
Quality and Quality Data AwardHealth Current |
 |
Government Relations and Advocacy AwardCyncHealth |
 |
Leadership AwardJill Eisenstein, Former CEO and President, Rochester RHIO |
 |
Emerging Leader AwardBeth Anderson, President & CEO, VITL |
 |
Board Chair AwardWaldo Mikels-Carrasco, Director of Community & Governmental Solutions, IHE |
 |
The Future of HIEs in the Rapidly Evolving Healthcare Market

- Date: Tuesday, August 17, 2021
- Presenter: Niam Yaraghi, PhD, Assistant professor of Business Technology at the University of Miami and non-resident fellow at the Brookings Institution’s Center for Technology Innovation
- Overview: Dr. Niam Yaraghi has worked closely with HEALTHeLINK in New York over the past 11 years to conduct important research into HIE adoption and evolution. Dr. Yaraghi provides his thought-provoking forecast for HIEs and suggests opportunities for HIEs to consider outside of traditional healthcare markets to support long-term sustainability. Futurist thought leadership is presented with ties to real-life observations about trends occurring in parallel, and sometimes unexpected, industries.
Dr. Yaraghi began working with HIEs while working on his PhD dissertation at SUNY about 11 years ago. As part of his work, he received an invitation from Dan Porecca to collaborate with HEALTHeLINK on his research interests. Over the years, Dr. Yaraghi published numerous articles about HIE business models and interactions between stakeholders in healthcare IT.
 Dr. Yaraghi opened his talk by highlighting the incredible acceleration in getting real solutions to market in the past year. He noted that, in many cases, we were likely on track to get these kinds of solutions and operational realities in a decade. The pandemic has accelerated that ramp-up time now to just a year. Examples include virtual meetings and healthcare visits.
Dr. Yaraghi opened his talk by highlighting the incredible acceleration in getting real solutions to market in the past year. He noted that, in many cases, we were likely on track to get these kinds of solutions and operational realities in a decade. The pandemic has accelerated that ramp-up time now to just a year. Examples include virtual meetings and healthcare visits.
Many of these changes are increasingly driven by forces external to healthcare as a service industry, such as changing reimbursement models, energy and pace dictated by venture capitalists, and the entry of new and competing retail-oriented vendors and solutions. Patients are also now demanding services that are flexible and convenient, not just available.
What makes these changes important is that, even though there might be slight usage reductions after a major event like the pandemic, their use becomes preferred, and many people are not willing to go back to older approaches. These rapid changes set a new point of equilibrium and redefine baseline expectations. Prior to the pandemic, many people had a hard time imagining switching more permanently to virtual care. When they were forced to, many found it more convenient, and it will be hard to take that convenience away from them. Providers can feel the same way when solutions augment care and make it easier for them to deliver care on a more regular basis. For example, some patients who might have had an aversion or logistical challenges in seeing doctors regularly might not find virtual visits appealing and are more likely to engage with their providers more proactively, willingly, and regularly. These can be good changes for many. Virtual visits do not mean losing personal connections either; it just means patients and providers are interested in more convenient and effective ways of working together.
Investments in technology have quadrupled in the past several years. Tech innovators and investors tend to have a different culture and energy when it comes to moving solutions to market, and this is having an effect on HIEs and the healthcare space. We are seeing rapid development of apps, wearables, and other solutions that are driven again by demand from consumers and the willingness of investors and innovators to rapidly respond to that demand. In many cases, these outside actors are not willing to put up the historically slow pace of progress in healthcare. They will continue to push hard for faster change.
Dr. Yaraghi led the audience in an exploration of retailers such as Walmart, Costco, and other market influencers and the amount of data they collect about customers. This data is collected not only during a purchase but also from customers’ behaviors, facial expressions, preferences, what they are and aren’t willing to do. Because of this demand for data and the growing ubiquity of ways of collecting it, there is no reason to think that outside organizations could not bypass HIEs in the collection of patient information. Walmart is already rolling out clinics, and other companies are poised to do similar things.
This week’s conference provides an example of a starting point that HIEs should think about to differentiate themselves from would-be competitors. For example, to attend this year’s conference, everyone needed to use the CLEAR app to attest to their vaccination status. As Dr. Yaraghi explained, this app did not include true verification but had a reliance on users taking a snapshot of proof of vaccination and entering some basic information. The world has its share of less than trustworthy actors, and in this one example, he did not think it would take much to forge a vaccination card and falsify information to gain admission to events like these. This is worrisome but is also an opportunity for HIEs to begin to look at certifications and independent verifications as a service.
 HIEs are in a position to partner with unique stakeholders going forward, including for-profit companies, hotels, sports and event venues, and the like. Other ideas include partnering with grocery stores to help nudge shoppers toward healthier options based on their medical conditions or developing partnerships with companies like Apple to push reminders to people’s phones or watches to take their medications at certain times. These will take some work but would be quite useful.
HIEs are in a position to partner with unique stakeholders going forward, including for-profit companies, hotels, sports and event venues, and the like. Other ideas include partnering with grocery stores to help nudge shoppers toward healthier options based on their medical conditions or developing partnerships with companies like Apple to push reminders to people’s phones or watches to take their medications at certain times. These will take some work but would be quite useful.
In Dr. Yaraghi’s view, HIEs have tended to serve as something more of a phone company—routing calls between two or a small number of parties. He posed the question: Why not be more like a Google? Why not be more for more stakeholders?
HIEs have a strategic advantage in their combination of medical data from difficult or impossible sources that most other sources cannot replicate and the trust they have developed with their stakeholders. Dr. Yaraghi noted, however, that one of the measuring sticks he uses to look at organizations’ preparedness for these kinds of futures is, simply enough, the number of data scientists they hire. In looking at current job postings from HIEs, he did not see many listings.
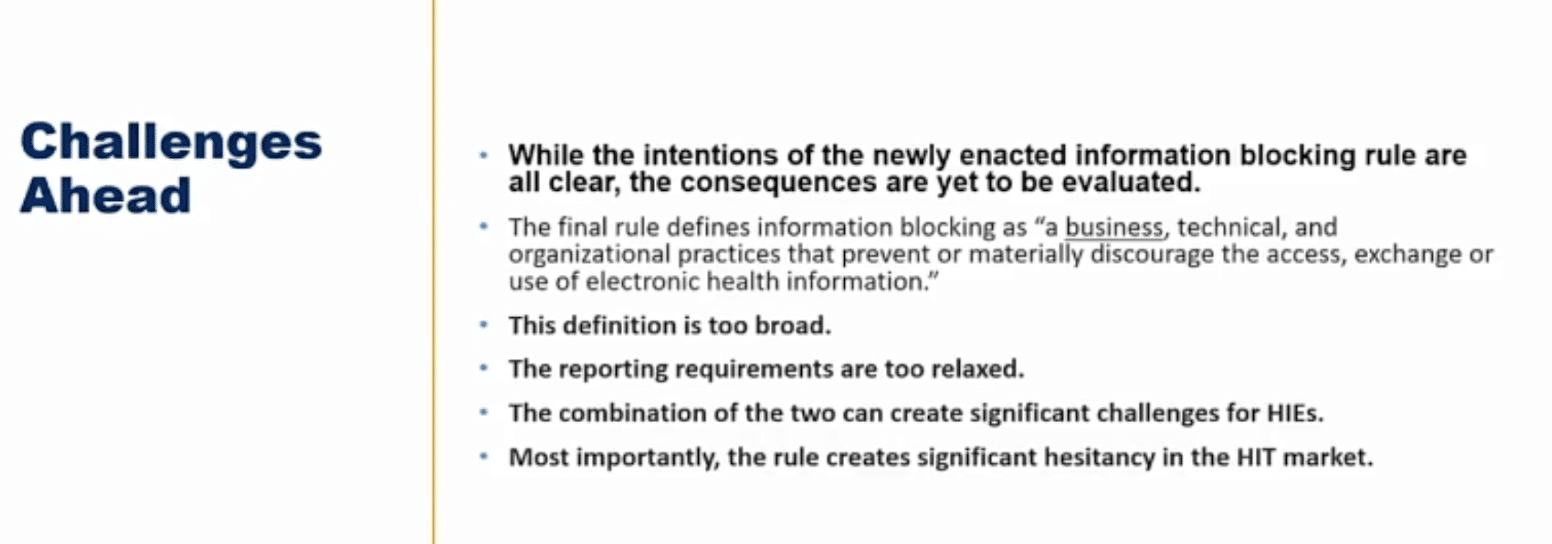
Dr. Yaraghi spoke briefly about the need for policy change and the degree of limitation placed on HIEs and the market at the federal level. He gave the example of information blocking rules. While good in theory, there is far too much latitude for anyone to file complaints, which can be unnecessarily costly to organizations, especially if there was no true blocking. The cost of having to go through the investigations and the publicity costs of being named in one can be significant and can erode one of the most valuable things an HIE has: trust.
Dr. Yarahgi took input from attendees. Some comments pertained to whether companies like Walmart would really only be concerned about getting people into their clinics to then sell them products. Potentially yes, but this should be weighed against the fact that over 90% of Americans live within five miles of a Walmart and would have better access to affordable basic services), to the fact that Dollar General recently hired a CMO and that Google makes it a policy to only venture into spaces where something is likely to be used on a daily basis.
The session concluded with Dr. Yaraghi highlighting his impression that real solutions are not likely to be at the EHR level. Their interests are too narrow. As an industry, HIEs need to think much more broadly, perhaps even to the very controversial level of charging patients for access to data products and services. After all, if we imagine HIEs to be utilities, don’t consumers pay utility bills?
Innovative Solutions to Unconventional Challenges: A Statewide Approach for Coordinating Healthcare Utilizing a Resource Engine

- Date: Tuesday, August 17, 2021
- Presenters:
- Nat Louden, Program Coordinator, Kentucky Health Information Exchange
- Andrew Bledsoe, Deputy Executive Director, Kentucky Health Information Exchange
- Judy Theriot, Kentucky Medicaid Medical Director, Cabinet for Health and Family Services
- Overview: Panelists discuss mandated participation at the state level in Kentucky has created positive outcomes in response to the COVID-19 pandemic.
Kentucky is one state where mandated participation at the state level has created dramatic results in response to the pandemic. Andrew Bledsoe, Deputy Director of the Kentucky Health Information Exchange (KHIE), explained that prior to COVID-19, KHIE had not worked with laboratories for the direct exchange of data. Today, they have connections with over 300 labs. In Kentucky’s case, the state-mandated participation has been critically important to the HIE’s ability to respond to data needs.
 Nat Loudon, KHIE’s Program Coordinator, described the HIE’s Social Determinants of Health (SDOH) program. SDOH is increasingly recognized as a vital part of understanding health and wellbeing—or the barriers that contribute to degrading it. Loudon presented slides showing Kentucky as one of the “dark spots” on the U.S. map, meaning lower economic stability, especially in southern and eastern portions of the state.
Nat Loudon, KHIE’s Program Coordinator, described the HIE’s Social Determinants of Health (SDOH) program. SDOH is increasingly recognized as a vital part of understanding health and wellbeing—or the barriers that contribute to degrading it. Loudon presented slides showing Kentucky as one of the “dark spots” on the U.S. map, meaning lower economic stability, especially in southern and eastern portions of the state.
Loudon linked economic status, education, community, and geography with chronic disease, heart disease, diabetes, and cancer. The take-away was that a large portion of Kentucky is at high risk for poor health.
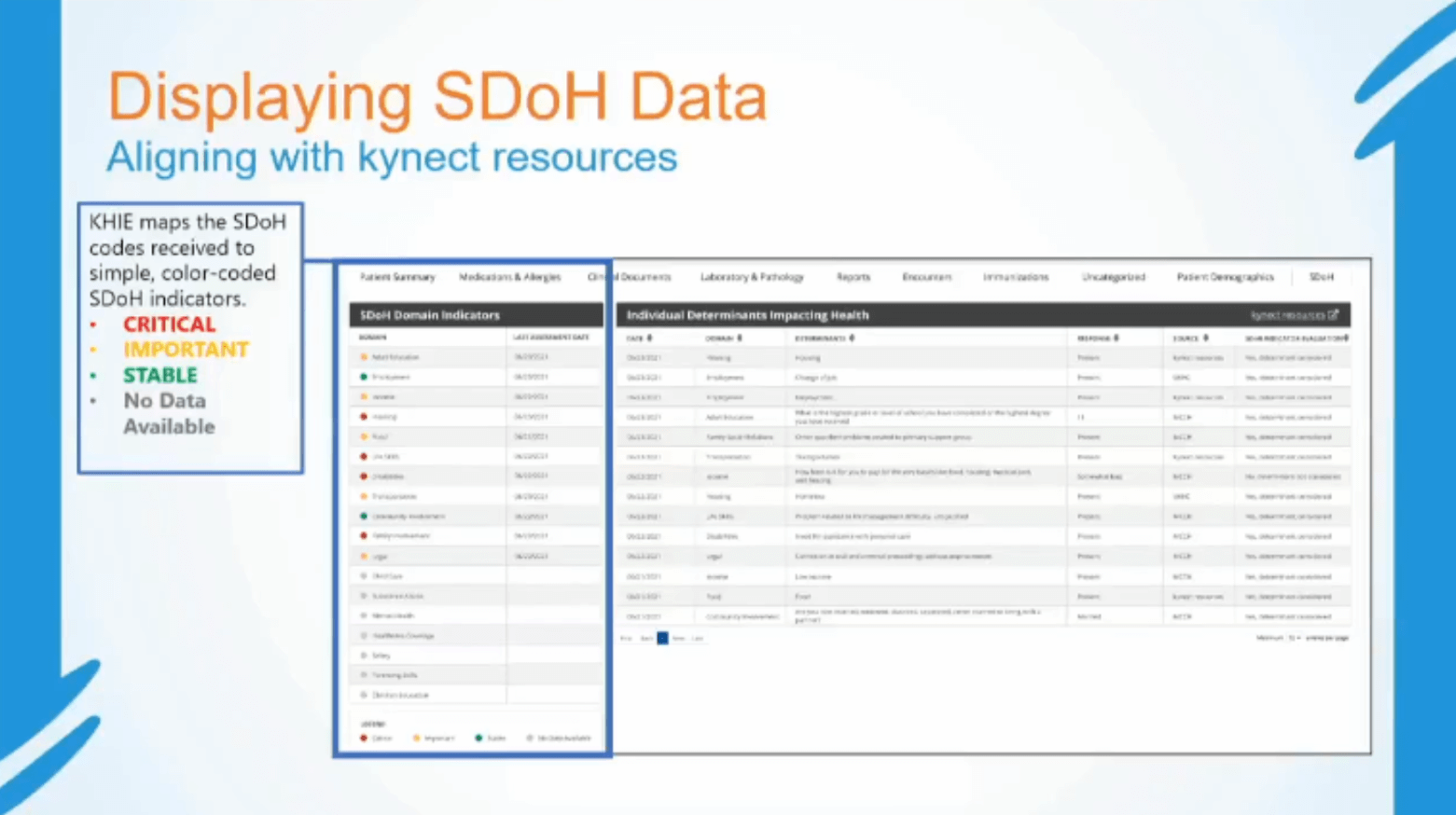
KHIE has collaborated with Kentucky’s kynect resources as a social care referral network and resource engine. Kynect is supported by the United Way’s 2-1-1 program, as well as state and community organizations.
Typically, people are affected by multiple determinants of health. Loudon noted significant overlays between unemployment, education level, and obesity in Kentucky’s southern and eastern counties. In many of these counties, Loudon found up to 40% unemployment and a high percentage of less than high school education.
KHIE now has a bidirectional connection with kynect resources. Each partner provides the following:
KHIE:
- Provider Evaluation: Residents’ SDOH indicators are evaluated, and SDOH codes are triggered and sent to KHIE’s ePartnerViewer and kynect resources.
- KHIE ePartnerViewer: Displays SDOH status within the viewer as either critical, important, or stable, providing participants actionable information to mitigate factors negatively affecting patients’ health.
- Referral Link: KHIE provides a referral link to kynect resources, bridging the gap between patient health information and available community resources.
Kynect resources:
- Needs Assessment: Residents complete a Needs Assessment to identify SDOH, which populates the resident’s records.
- Kynect resources: A web-based portal connects residents to over 10,000 affordable and accessible community resources across the state. Real-time SDOH domain indicators are available on a resident’s profile within the portal.
To augment basic connectivity and information sharing, KHIE developed an in-house tool that aligns or maps SDOH data found in ICD-10 and LOINC 80216-5 codes to the kynect resources Needs Assessment.
Loudon’s slides showed screen captures of the visual display, including the easy-to-interpret color-coded severity indicators and an intuitive UI for users to see both a summary view of contributing factors and details to understand how those determinants have influenced health status.
The goals of the SDOH initiative and collaboration with kynect resources have been to put available SDOH data to actionable use (not just display static data), encourage the use of existing community resources and aid in navigating those resources, and increase direct patient engagement. KHIE hopes that these tools will improve patient outcomes, population health, and incentives for new SDOH-based research.
Bledsoe returned to the podium to talk about KHIE’s advancements in providing PACS images to support clinical decision-making. While, in many cases, providers do not need to see full images, KHIE has invested in the technology to provide both “thumbnail” views of images and full images for those who need them.
Dr. Theriot noted that from a pediatrician’s perspective, the full images might not be necessary on a routine basis, but viewing the lower-quality images helps in a range of work, including conversations with parents to help them visualize what is being discussed about diagnoses affecting their child.
According to Bledsoe, KHIE determined that it cost approximately $25, on average, to produce each of the imaging discs traveling around to providers. At one facility alone, the total cost of producing these discs was six figures per year—and creating them did not guarantee that providers received the discs in a timely manner.
Bledsoe shared a story about his wife needing a second image because a “second opinion” facility could not access the original images in a timely manner. They found out after the fact that their insurance did not cover the second set of images.
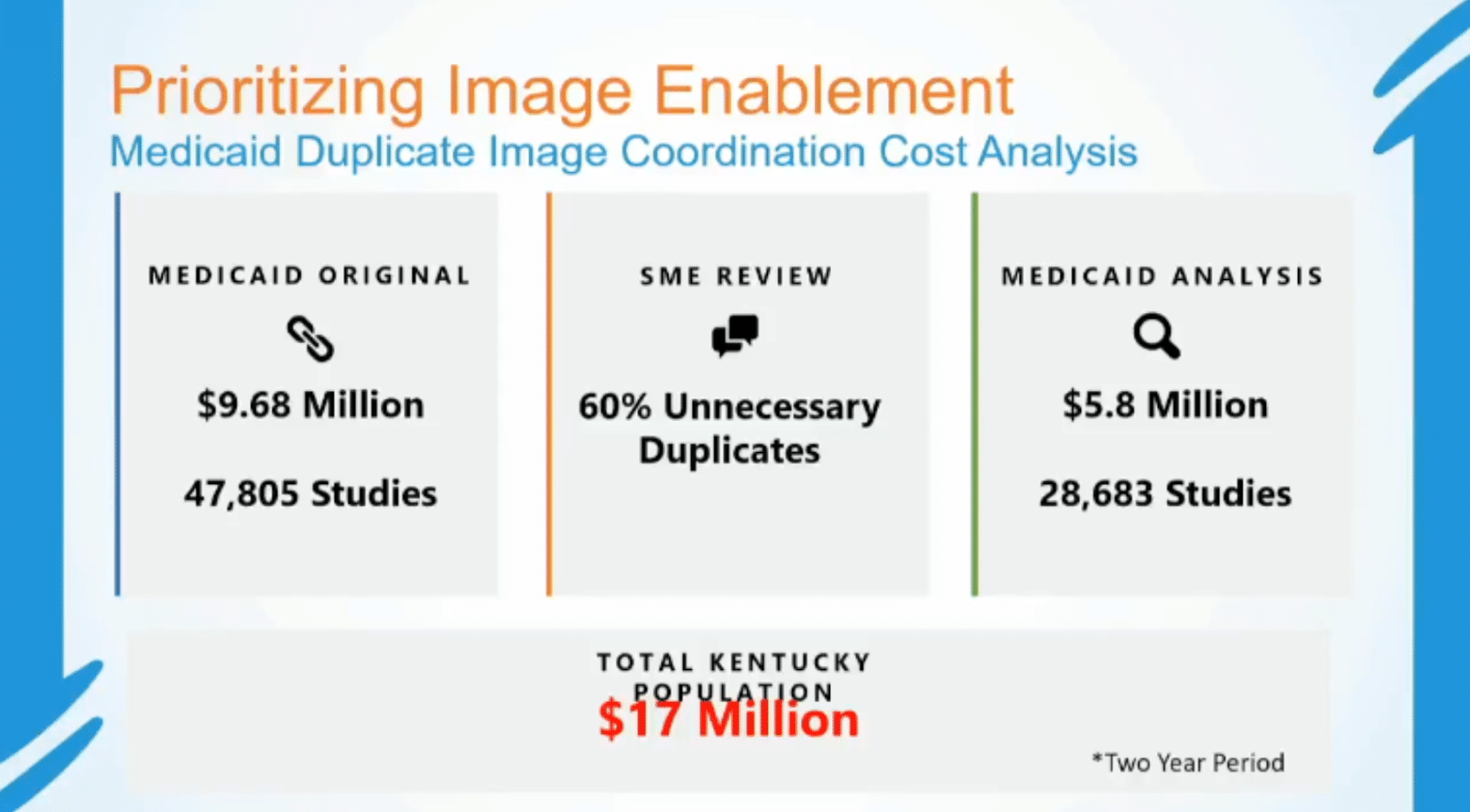 Dr. Theriot shared slides showing investigations into the Medicaid population, specifically, and costs associated with potentially unnecessary duplicate imaging. Medicaid, by law, can only cover indicated services. In total, over a two-year period, Theriot found that $5.8 million in Medicaid imaging (28,683 studies) was unnecessary, meaning 60% of duplicate images were also unnecessary. When extrapolated beyond Medicaid, Theriot showed an estimated $17 million in unnecessary duplicate imaging in Kentucky in the same time period.
Dr. Theriot shared slides showing investigations into the Medicaid population, specifically, and costs associated with potentially unnecessary duplicate imaging. Medicaid, by law, can only cover indicated services. In total, over a two-year period, Theriot found that $5.8 million in Medicaid imaging (28,683 studies) was unnecessary, meaning 60% of duplicate images were also unnecessary. When extrapolated beyond Medicaid, Theriot showed an estimated $17 million in unnecessary duplicate imaging in Kentucky in the same time period.
These, of course, are just the dollar costs. There is also the time cost and, most importantly, the excess exposure to radiation.
KHIE’s use of their ePartnerViewer to enable electronic access to images is expected to dramatically reduce all of these forms of waste for Kentucky and serve as a useful model for other HIEs exploring the value of investing in electronic image sharing capabilities.
To fund their Image Exchange solution, KHIE is leveraging HITECH funding through September 2021. KHIE is requesting Medicaid Management Information System (MMIS) funding for operations and onboarding beyond September 2021.
Audacious Goals, Alliances for Action, and Amazing Leadership


- Date: Tuesday, August 17, 2021
- Presenters:
- Jaime Bland, CEO, CyncHealth
- Jess Kahn, Partner, McKinsey & Company
- Kat McDavitt, Principal Advisor & Public Affairs Practice Head, Insenna Communications
- Carrie Paykoc, Director of the Office of eHealth Innovation, State of Colorado
- Melissa Kotrys, CEO, Contexture | Board Chair, SHIEC Board of Directors
- Overview: Speakers discuss public-private partnerships and examples of the types of compromises and prioritization in which HIEs need to engage to demonstrate progress toward greater sustainability and recognition as an essential resource to state and local officials.
Felicia Quintana-Zinn and Jaime Bland began by speaking about the relationship between the state’s Department of Health and Human Services and CyncHealth, Nebraska’s statewide HIE. Both agreed that in the beginning, finding common ground was difficult. Their relationship began as a legislative mandate. After a number of discussions, they concluded that while their ideas about how to get to specific outcomes differed, they did at least agree on those outcomes. Finding this point of connection allowed them to continue to work through differences of thought to find compromises and paths forward.
Panelists discussed the criticality of building bridges for partners, which means advocating for partners like state departments and agencies in discussions with local or private stakeholders to help increase awareness about goals, needs, and abilities.

Jess Kahn commented on the importance of a convener management style and how the approach of nurturing relationships has been so important to the progress for HIEs and state and local partners in the last few years.
Bland shared her background in nursing. When she started with the HIE less than four years ago, she was struck by the level of what seemed like head-to-head competition. She noted the evolving tone—what some have been referring to as more of an environment of “coopetition.”
Panelists also shared their gradual shifts from thinking they needed to solve all of their respective organizations’ problems internally, separately, or with private commercial solutions, to a mental model and culture that routinely asked questions like “can we solve this with the help of any of our partner organizations?” or “do we have partners who can do this better or faster than we can?”
There is still work to be done in completing this shift in mindset, but the panelists all seemed to agree they were heading in the right direction.
The panelists also called attention to the need to develop deeper relationships within organizations. The average lifespan of a Medicaid director, for example, was said to be about 18 months. Appointed and high-pressure positions might see a lot of turnover, which underscores the importance of nurturing relationships at multiple levels of an organization. This turnover also tends to mean finding the people who are committed to making change, whatever their title. Titles can be misleading or not representative of the influence a particular person might have. A lot of this influence has to do with how driven an individual is and how passionate they are about change. The group felt that finding these people and sticking with them is one of the best uses of time when it comes to relationship-building.
Where states are fortunate to have long-standing leaders in key roles (such as in Arizona; only three Medicaid directors in ten years), HIEs should leverage these relationships to ask for support, take action on shared ideas, and work on keeping communication lines as open as possible. For these HIEs, having easy, frequent, and open conversations with what grow to become well-respected colleagues in partnership organizations can make a world of difference in an HIE’s quest to be recognized as essential.
Where states have high turnover among social care organizations, government offices, and other key stakeholders, telling the same story many times may be necessary. Nevertheless, these are the conversations that move HIEs forward and, aside from government mandates that drive action, there are not many reliable substitutes. People need to talk and do so more openly.
When conversations become stymied in one place, such as at the state level, having a broad network among community organizations, providers, and other leaders in a community can often lead to breakthroughs.
Panelists talked about the need for more representation from states and local governments at events like this one in the future. Bringing more people to the table is better than working in relative isolation wondering if someone else is thinking the same thing.
In discussing approaches that seem to work best, both public and private industry representatives on the panel agreed that the key for HIEs is to do an even better job of really listening. What doesn’t work is going into meetings with an agenda to push or things to sell. Listen first.
Panelists fielded a few questions, including how they saw the next three to five years shaping up. Most, aside from interpersonal skills and relationship-building, talked about the need to focus on optimizing the value of data and stitching data together from new sources. These new data sources can include WICC, claims data (if they do not use it already), court data for mental health support, linking Medicaid assessments to child care services, and the like.
The panel generally felt that there is still too much fragmentation and vendors with specific niches that they are willing to fill. Jess Kahn, for one, felt that it is the government’s job to provide both incentives and guardrails within which innovation can occur. Leaving it entirely open-ended or putting in place too many penalties for being creative leads to fragmentation.
Felicia Quintana-Zinn helped to wrap up the discussion by offering advice to HIEs: Ask your partners what their gaps are and find ways to help them. Generally, they are going to be glad that you are taking an interest and will share insights that might lead you in a more meaningful direction.
Thank you for joining us for day two at SHIEC!
| Day One Summary | Day Two Summary | Day Three Summary |
|---|
J2 Interactive is an award-winning software development and IT consulting firm specializing in customized solutions for hospitals, labs, research institutions, and health information exchanges.
Our approach to design and development is rooted in a fundamental belief that systems succeed or fail based on how well they serve the people who depend upon them. Drop us a line to learn more.



