The session showcased how CRISP DC’s Health Information Exchange (HIE) infrastructure, in collaboration with DCPCA and other local healthcare providers, is advancing whole-person care initiatives across the city. The discussion focused on how partnerships and public-private collaboration are driving the development of analytics tools that address both clinical and social needs.
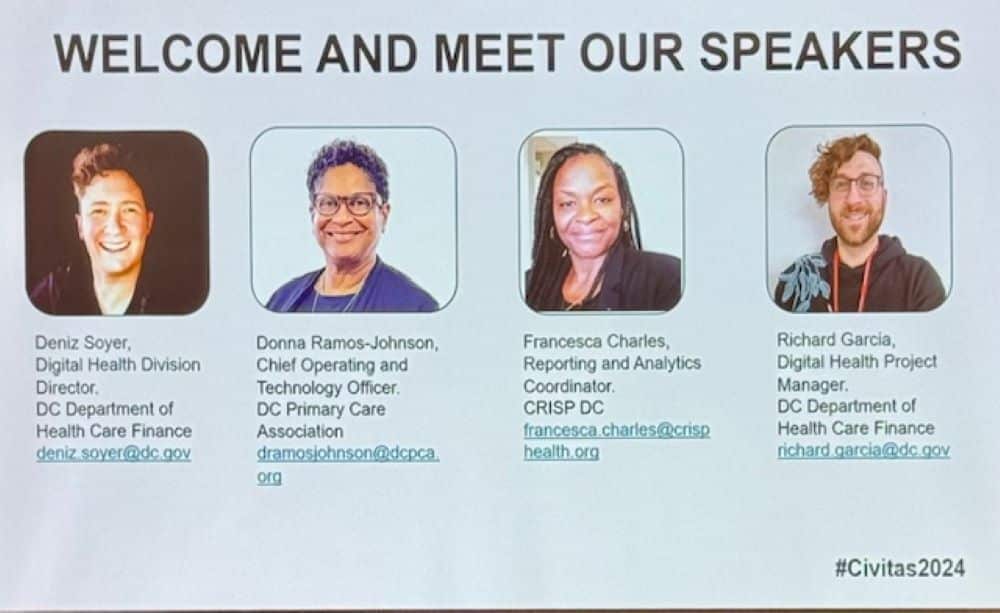
Deniz Soyer, Digital Health Division Director at DC’s Department of Health Care Finance, explained that HIE infrastructure is not just technology—it serves as the backbone for connecting stakeholders, sharing data across sectors, and driving value-based care initiatives. The collaboration between providers, CRISP, and community organizations helps overcome fragmented care by linking administrative, clinical, and social data streams, ensuring care is more cohesive and responsive.
The panel emphasized the importance of Population Navigator, a tool developed through collaborative input from FQHCs, providers, and CRISP DC. This tool gives providers access to detailed patient lists segmented by conditions, recent visits, and care needs, such as diabetes care or hospital readmissions. With this tool, healthcare teams can generate targeted reports to better understand utilization trends and develop specific outreach strategies. Providers can also use heatmaps to visualize patients’ social needs, like food insecurity or homelessness, enabling timely and tailored interventions.
Donna Ramos-Johnson of DCPCA highlighted the technical assistance program they offer to smaller practices and FQHCs, ensuring that all providers—regardless of size—can connect with and leverage the HIE effectively. This support ensures that providers not only engage with tools like Population Navigator but also contribute feedback for continuous improvement. Through ongoing feedback loops, CRISP DC customizes analytics and reporting to align with the needs of its users, creating dashboards that reflect real-world challenges.
The session also noted that z-codes and ADT messages (admission, discharge, and transfer) are critical in capturing social needs within the HIE, such as housing instability or financial insecurity. This data helps providers identify patients with unmet needs and coordinate care plans across providers and managed care organizations (MCOs). Francesca Charles of CRISP DC emphasized that these partnerships ensure transparent data sharing, fostering trust between providers and enabling predictive modeling and risk stratification—paving the way for value-based payment models.
As the first jurisdiction in DC to adopt Medicaid Enterprise Systems (MES) in 2021, DC’s progress serves as a replicable model for integrating cross-sector partnerships with HIEs to address population health needs. The public-private partnerships discussed in the session demonstrate that collaborative approaches—coupled with advanced data tools—can help overcome fragmented care and improve health outcomes.



